A compression fracture is a break in a vertebra (a bone in your spine). When broken, this bone collapses. These spinal fractures are common as you age, or they happen due to osteoporosis. Over time, vertebral fractures cause your spine to curve or collapse. Treatment includes rest, medications, braces and minimally invasive surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
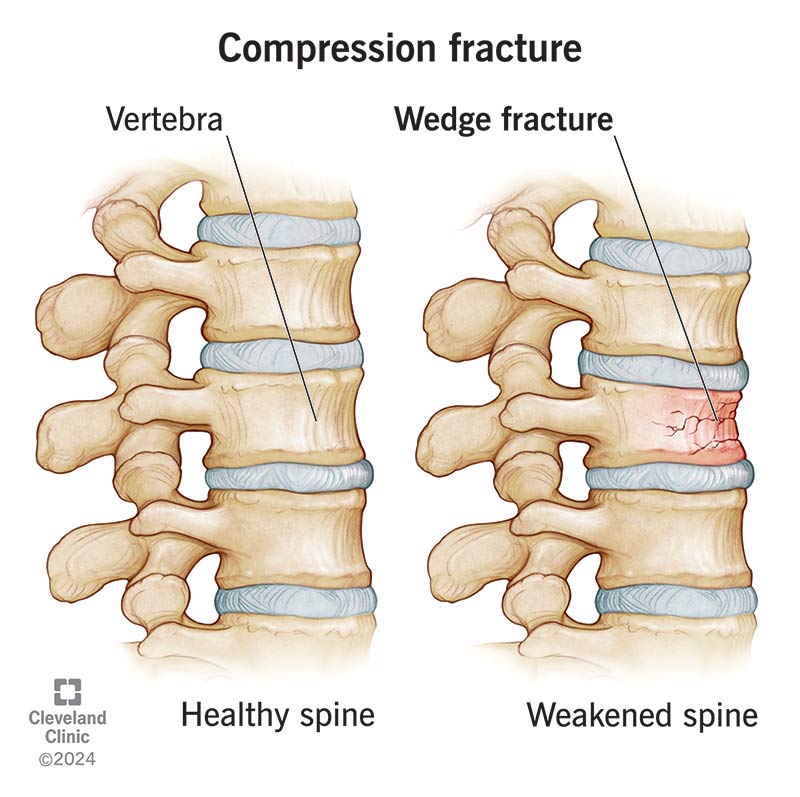
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21950-compression-fractures)
Compression fractures are small breaks or cracks in the vertebrae (the bones that make up your spinal column). The breaks happen in the vertebral body, which is the thick, rounded part on the front of each vertebra. Fractures in the bone cause your spine to weaken and collapse. Over time, these fractures can affect your posture.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Compression fractures can happen to any part of your spine, but they usually occur in the thoracic spine (middle section). Osteoporosis is a common cause of compression fractures, in addition to trauma (like after an accident) or tumors that weaken the bone.
A healthcare provider may treat these fractures with medications, a back brace or surgery, depending on the cause and severity of the bone break.
You may hear your provider refer to a compression fracture as:
The types of spinal compression fractures include:
Compression fractures are either:
Advertisement
Compression fractures are common. An estimated 1 to 1.5 million compression fractures happen every year in the United States.
The symptoms of a compression fracture may include:
Compression fracture symptoms range from mild to severe. You may not notice or feel symptoms with mild fractures.
A common sign of a compression fracture is a loss of height. The fracture causes the bone to collapse, which may affect how tall you are.
Pressure on or against the vertebrae in your spine may cause your spinal bones to break and collapse. Some of the most common causes of a compression fracture include:
You may be more at risk of a compression fracture if you:
Studies show that an estimated 40% to 50% of people aged 80 or over experienced a compression fracture before.
Long-term complications of a compression fracture may include:
To diagnose a compression fracture, your provider will offer a physical exam to learn more about your symptoms. During the exam, your provider:
Your provider will also recommend imaging tests to see pictures of the bones, muscles and soft tissues in your back. These imaging studies include:
Advertisement
In some cases, your provider may find a compression fracture while performing an imaging test for another reason.
Compression fracture treatment focuses on:
Depending on the type and severity of the fracture, treatment may include:
Yes, some types of compression fractures can heal on their own. Healing can take several months. A healthcare provider may offer treatment options like a brace to make sure your spine heals as expected. Let your provider know if you have symptoms that interfere with your daily routine and mobility as you heal.
Advertisement
Your outlook after a compression fracture varies based on:
Many compression fractures heal after a few months of rest and limited movement. If symptoms are bothersome, a healthcare provider may offer different treatment options to relieve pain.
If you have osteoporosis, you have a higher chance of having another compression fracture. Your provider can help you manage osteoporosis to prevent future fractures.
As your spine bones heal, you may notice symptoms like pain decrease after about four weeks. It should completely heal after 12 weeks. Your age and other factors may affect your healing time.
A compression fracture is only one factor that helps calculate your life expectancy and it isn’t the only thing your provider will consider. For example, a first-time vertebral compression fracture may indicate to a provider that osteoporosis is progressing and taking a greater toll on your body, even if you’re in otherwise good health.
Know that your situation may or may not fit statistics. Your provider can give you the best information about what you can expect.
You can’t prevent all causes of compression fractures.
Advertisement
One of the most common causes is osteoporosis. To reduce your risk of an osteoporosis-related compression fracture, you should:
Visit a healthcare provider if you have sudden back pain or other symptoms of a compression fracture that doesn’t resolve in a couple of days. It’s especially important to stay regular with visits to see your provider if you have osteoporosis.
Contact emergency services or visit the emergency room if you have sudden, severe back pain and:
If you have a compression fracture, you may want to ask your provider:
No one wants a broken bone, especially a break in the bones that support your body and help you sit, stand and move. Compression fractures — small breaks or cracks in the vertebrae — come with symptoms like pain and discomfort, which may take you out of some of your favorite activities for several weeks.
These fractures are common and not always preventable. But there are steps you can take to reduce your risk, like removing tripping hazards from your living space or wearing a seatbelt when riding in a vehicle. Your provider may have more suggestions specific to you and your lifestyle.
When healing from a fracture, don’t rush this process. It could extend your recovery time or lead to complications. Be sure to follow your provider’s instructions carefully so you can heal properly.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Back pain can stop you in your tracks. But you don’t have to live like that. Cleveland Clinic is here to help you get moving again.
