Tracheal stenosis happens when you have inflammation or scar tissue in your trachea that makes your trachea narrower. The tighter airway makes it more difficult for you to breathe. It can be acquired during your lifetime or present at birth. The most common treatments are procedures that stretch your trachea or surgeries that reconstruct it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
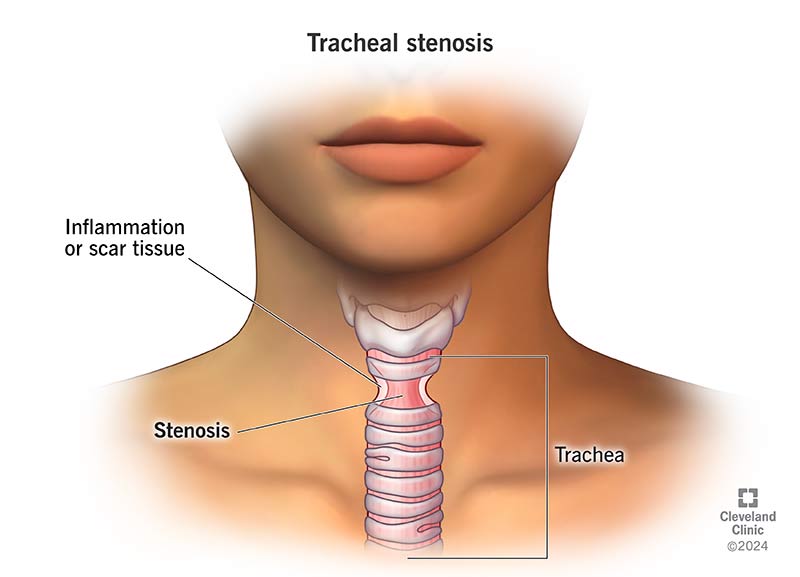
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/21866-tracheal-stenosis)
Tracheal stenosis involves narrowing of your trachea (windpipe) that makes it harder to breathe. Your trachea is a tube made of cartilage and soft tissue. Air travels through your trachea on the way from your nose and mouth to your lungs. When you have tracheal stenosis, inflammation, injury or scar tissue in your trachea makes it harder for air to flow through.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Stenosis” is the medical term for atypical narrowing in a body passage. It can develop in different parts of your throat. For example, a related condition called laryngotracheal stenosis involves narrowing in both your trachea and larynx (voice box). Subglottic stenosis is narrowing in the area above your trachea and below your vocal cords.
Regardless of the part of your throat that’s affected, you should contact a healthcare provider if you’re having difficulty breathing.
There are two types of tracheal stenosis:
Tracheal stenosis is life-threatening in infants. Seek emergency care if your newborn is showing signs of tracheal stenosis, like struggling for air.
That said, both forms of tracheal stenosis make it harder to breathe, which can affect your quality of life. That’s why seeing a healthcare provider is so important if you or your child has this condition.
Advertisement
Many tracheal stenosis symptoms are the same for children and adults. Common symptoms include:
Children are more likely to have additional symptoms:
With congenital tracheal stenosis (CTS), the cartilage that makes up an infant’s trachea doesn’t form correctly, causing their windpipe to be too narrow.
Long-term intubation is the most common cause of acquired tracheal stenosis. Intubation is a lifesaving treatment that involves inserting a tube into your trachea so you can breathe. Sometimes, intubation causes damage that leads to stenosis. Children may develop tracheal stenosis if they were born with premature lungs and their provider used breathing tubes to help them get air.
You might also develop tracheal stenosis if you:
Otolaryngologists (ENTs) use several tests to diagnose tracheal stenosis and decide how to treat it. Tests may include:
Advertisement
You may need other tests to check for what’s causing your condition. Tests may include a blood test to check for inflammation or infection or a biopsy to see if unusual growths in your airway are cancerous.
Surgeries and procedures that widen your trachea are the most common treatments for tracheal stenosis. Treatment options include:
The best treatment for tracheal stenosis depends on lots of things, including where the narrowing is and how severe it is. Your provider will explain how these factors inform which procedures will work best for you.
Advertisement
You’ll likely need surgery or a nonsurgical procedure if you have tracheal stenosis. Each treatment option has different recovery times and outcomes.
For example, tracheal resection and reconstruction surgeries are invasive. But they’re more likely to eliminate the narrowing in your trachea in the long term. Nonsurgical procedures, like tracheal dilation, are less invasive. They may be the only treatment you need, or you may repeat procedures.
Regardless of the procedure, your healthcare provider will monitor you to check for recurrence. Tracheal stenosis sometimes comes back because treatment can cause new scar tissue to form. Your provider will explain how likely it is that your condition will return.
You might start by asking your healthcare provider how your surgery will affect you. Every procedure to treat tracheal stenosis will require different at-home care. Your healthcare provider will have information about your next steps. They may advise you on:
Advertisement
Your healthcare provider will schedule follow-up appointments to check on your recovery after treatment. At first, you may need to see your provider every few weeks or so. If you’re healing well, your provider may extend follow-up visits to every few months until they’re confident the stenosis won’t return.
Contact your provider anytime you’re experiencing shortness of breath. While next steps vary depending on your condition, it can be dangerous to put off getting help when you’re having difficulty breathing. It’s essential to seek care.
You should go to the emergency room if you can’t breathe or have other tracheal stenosis symptoms. The symptoms might be a sign your tracheal stenosis has come back.
If you’re caring for a newborn or infant who’s having difficulty breathing, get them to an emergency room immediately.
If you develop tracheal stenosis, you might want to ask your healthcare provider the following questions:
Tracheal stenosis is often a complication of intubation — a lifesaving treatment that helps you breathe in an emergency. If you’re experiencing breathing difficulty after intubation, reach out to your healthcare provider. There are treatments available that can help. Talk to your healthcare provider about your options to ease your symptoms so that you can breathe freely.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic has a specially trained team for tracheostomy care and removal. Our compassionate healthcare providers keep you safe, comfortable and prepared.
