Salter-Harris fractures are cracks in a child’s growth plate — the special section of cartilage at the ends of their long bones. They only affect kids and teens because growth plates harden into regular bone when a child is done growing. Providers treat most growth plate fractures with casts. They usually heal in around a month.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
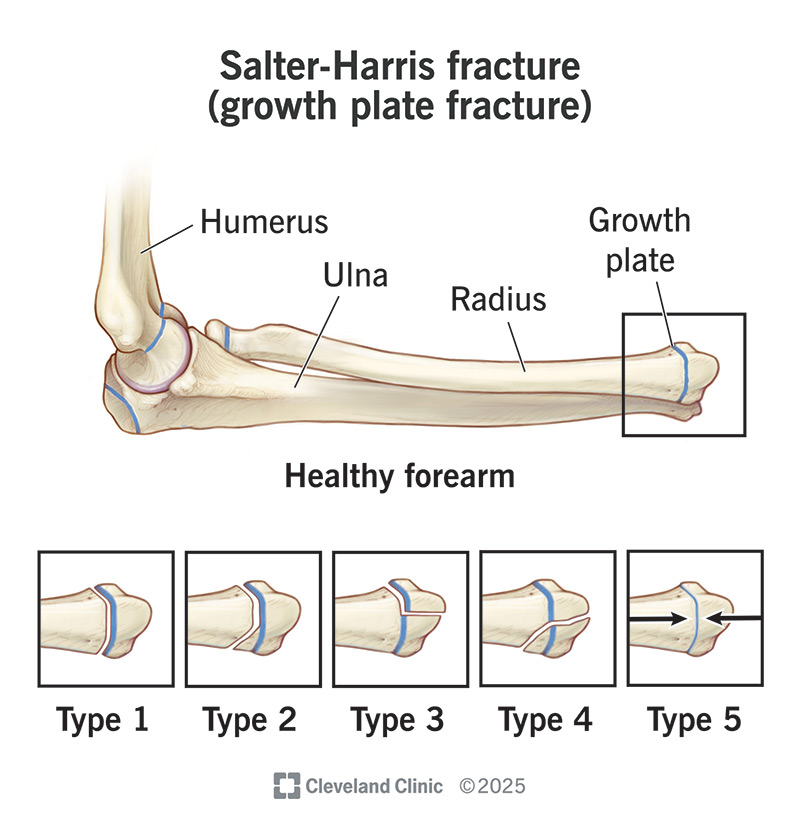
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/salter-harris-fracture-growth-plate-fracture)
A Salter-Harris fracture is a type of broken bone in a child’s growth plate. That’s why it’s also known as a growth plate fracture.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The growth plate is a section of cartilage that kids and teens have at both ends of some bones, including the:
The growth plate is exactly what it sounds like. It’s a special piece that helps bones grow and develop into the correct size and shape. Growth plates harden into solid bone when a child has finished growing.
Visit a healthcare provider if your child has bone pain, swelling, or one of their body parts looks noticeably different or out of place. Most Salter-Harris fractures take several weeks to heal. It’s important to get them diagnosed and treated right away.
Salter-Harris fractures get their name from the classification system healthcare providers use to divide them into five types:
Advertisement
The most common Salter-Harris fracture symptoms include:
Younger children might not be able to tell you they’re injured or describe what they’re feeling. Look for your child suddenly favoring a part of their body. They might reflexively hold their injured limb close to their body, wince or limp.
Sudden traumas are the most common causes of growth plate fractures, including:
Overtraining or specializing too soon in one sport can put repetitive stress on your child’s growth plates. This can lead to a fracture. Children and teens shouldn’t play the same sport year-round until their bodies finish developing.
Any child can experience a growth plate fracture. But some are more likely than others, including:
Most growth plate fractures don’t lead to complications. That’s especially true if a healthcare provider diagnoses and treats them within a week of the original injury. Rare complications can include:
A healthcare provider will diagnose a Salter-Harris fracture with a physical exam and imaging tests. Your provider will examine the area around the injury. They might check whether your child can move part of their body. They’ll compare it to the other, uninjured limb.
Tell your provider anything you know about what your child was doing before the injury. This includes when you first noticed something was wrong or when they felt pain.
Your provider will use at least one type of imaging test to take pictures of your child’s bones and the other tissue around their injury. They might need:
Wearing a cast is the most common Salter-Harris fracture treatment. The cast will protect your child’s bone and hold it in the correct position while it heals. Your provider will tell you the type of cast your child will need. They’ll also tell you how you can help your child take care of it.
Advertisement
It’s rare to need surgery to repair a growth plate fracture. It’s more common with more severe fractures (types 3, 4 or 5).
If your child needs surgery, a surgeon will perform what’s called an internal fixation. They’ll realign your child’s bone. Then, they’ll put fasteners — like metal screws, pins or wires — in the bone to hold it in place while it heals.
Your child might need follow-up surgery to remove the fasteners after their bone heals. Your provider or surgeon will tell you what to expect.
Most kids need to wear a cast for around a month after a growth plate fracture (usually four to six weeks). It might take longer if they had a more severe type of fracture, or if they needed surgery.
Your provider will tell you what to expect. The healing time depends on which of your child’s bones was injured and the type.
Visit a healthcare provider right away if your child experiences trauma, like a severe fall or car accident.
Go to the emergency room if you think your child has a broken bone. And go to the ER if they’re experiencing any of the following symptoms:
Advertisement
Most Salter-Harris fractures heal without long-term effects on a child’s health and development. Getting a growth plate fracture diagnosed as soon as possible is the best way to reduce their risk of complications.
Ask your provider when it’s safe for your child to return to sports or resume physical activities. If your child’s growth plate hasn’t completely healed before they start putting stress on it again, there’s an increased risk of complications (including refracturing it).
It’s always scary when your child is hurt, especially if it happened during a fall or accident you can’t prevent. Growth plate fractures can be serious, but most kids bounce back just fine after they’ve had time to heal.
The most important part of treating a Salter-Harris fracture is time — visit a provider as soon as possible if you think your child has a growth plate fracture (or any other bone injury). The sooner your provider can diagnose the fracture and get your child in a cast, the faster they’ll heal up and be back to their usual routine and activities.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When your child breaks a bone, you might worry about what comes next. Cleveland Clinic Children’s orthopaedic specialists can help make a treatment plan.
