Cutaneous T-cell lymphoma is a group of rare blood cancers that affect your skin. Most cutaneous T-cell lymphomas grow very slowly and aren’t life-threatening. Rarely, people with cutaneous T-cell lymphomas develop serious forms of the condition. Healthcare providers have treatments to ease symptoms, but they can’t cure the lymphomas.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
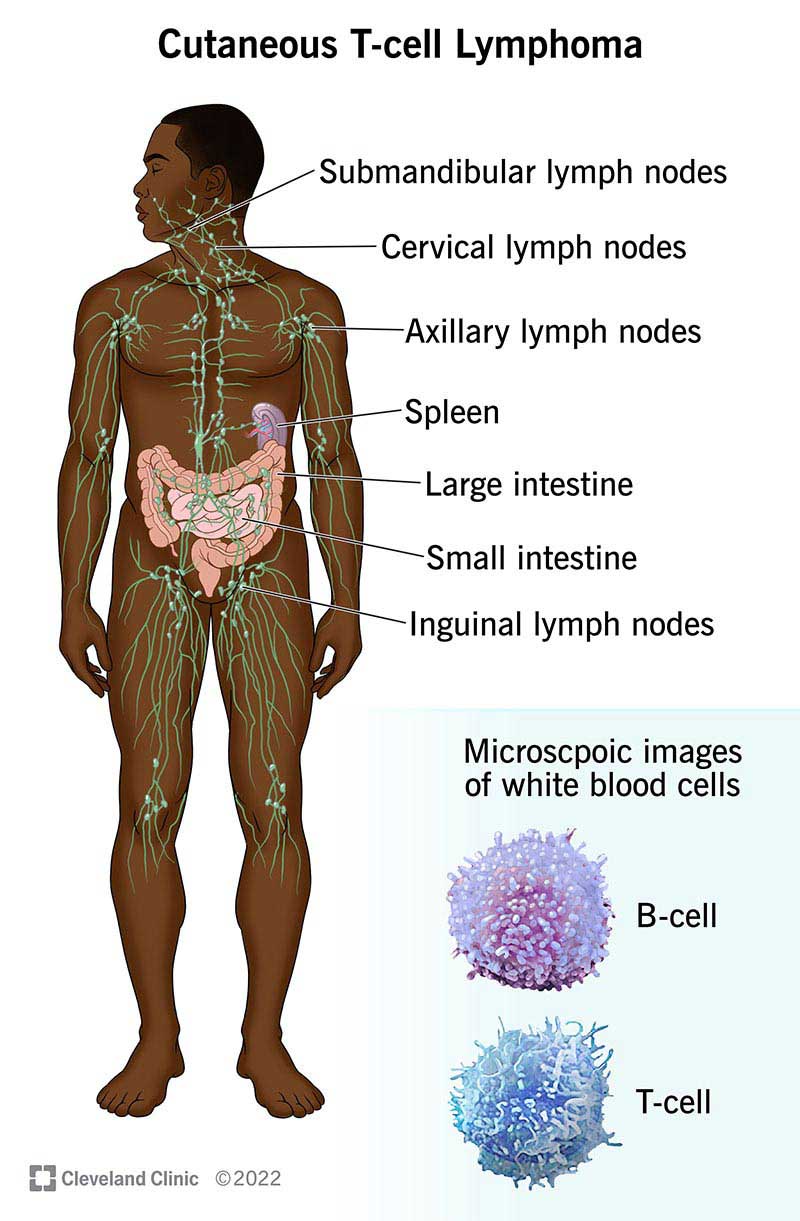
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/17940-cutaneous-t-cell-lymphoma)
Cutaneous T-cell lymphoma (CTCL) is a group of rare blood cancers that affects the largest organ in your body — your skin. CTCLs can look and feel like common skin conditions like psoriasis, eczema or even allergic reactions. Many people have symptoms like skin rash, itchiness or discoloration for years before obtaining a diagnosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
CTCLs are part of a larger group of cancers called non-Hodgkin lymphoma, which start in certain white blood cells called lymphocytes.
Many people treated for CTCL go into remission, returning to their daily routines without much disruption. Still, a cancer diagnosis can take a toll on your mental and emotional health. Your healthcare team is here to help.
There are many types of cutaneous T-cell lymphoma. But the most common are mycosis fungoides and Sézary syndrome:
Cutaneous T-cell lymphomas are rare. Healthcare providers estimate mycosis fungoides, the most common form of CTCL, affects 1 in 1 million people in the United States.
Advertisement
Symptoms of cutaneous T-cell lymphoma include:
In cutaneous T-cell lymphoma, T lymphocytes mutate (change) into cancerous cells that multiply uncontrollably. Healthcare providers don’t know exactly why CTCLs happen, or why some people are more likely than others to get them. Here are two possibilities:
You’re more likely to develop cutaneous T-cell lymphoma if you:
A healthcare provider will review your medical history and do a physical examination, focusing on any patches or plaques (thickened areas) on your skin. They’ll ask you about your symptoms and review your health history, including any prior or current health conditions.
Your healthcare provider will need to run tests to confirm a cutaneous T-cell lymphoma diagnosis. These tests may include:
Healthcare providers use staging systems to categorize, diagnose and treat cancers. The TNM classification system is the most common for staging CTCLs. This system describes:
The TNM system uses numbers and letters to stage cutaneous T-cell lymphoma:
| Stage of CTCL | Characteristics |
|---|---|
| Stage I (1)A | Discolored patches cover less than 10% of your skin. |
| Stage I (1)B | Raised, discolored patches cover more than 10% of your skin. |
| Stage II (2)A | You also have some swollen lymph nodes. You might have abnormal lymphocytes in your lymph nodes. |
| Stage II (2)B | You might have one or more skin tumors larger than 1 centimeter in size. |
| Stage III (3)A | Skin discoloration covers at least 80% of your body. You may or may not have swollen lymph nodes. Less than 5% of the lymphocytes in your blood are abnormal. |
| Stage III (3)B | You may or may not have swollen lymph nodes. Slightly more than 5% of the lymphocytes in your blood are abnormal. |
| Stage IV (4)A | Abnormal lymphocytes have spread to your lymph nodes or your blood. |
| Stage IV (4)B | The cancer has spread to other organs in your body, like your liver, lungs or bone marrow. |
| Stage of CTCL | |
| Stage I (1)A | |
| Characteristics | |
| Discolored patches cover less than 10% of your skin. | |
| Stage I (1)B | |
| Characteristics | |
| Raised, discolored patches cover more than 10% of your skin. | |
| Stage II (2)A | |
| Characteristics | |
| You also have some swollen lymph nodes. You might have abnormal lymphocytes in your lymph nodes. | |
| Stage II (2)B | |
| Characteristics | |
| You might have one or more skin tumors larger than 1 centimeter in size. | |
| Stage III (3)A | |
| Characteristics | |
| Skin discoloration covers at least 80% of your body. You may or may not have swollen lymph nodes. Less than 5% of the lymphocytes in your blood are abnormal. | |
| Stage III (3)B | |
| Characteristics | |
| You may or may not have swollen lymph nodes. Slightly more than 5% of the lymphocytes in your blood are abnormal. | |
| Stage IV (4)A | |
| Characteristics | |
| Abnormal lymphocytes have spread to your lymph nodes or your blood. | |
| Stage IV (4)B | |
| Characteristics | |
| The cancer has spread to other organs in your body, like your liver, lungs or bone marrow. |
Healthcare providers use several methods to treat CTCL, including:
Treatment is different for everyone. Your provider will let you know which options they recommend in your situation.
Most CTCLs grow very slowly and aren’t life-threatening. But some people develop serious forms of the condition. Healthcare providers can’t cure CTCLs, but they can successfully manage symptoms with treatment.
But like all cancers, CTCLs can be fatal in their advanced stages. The sooner you start treatment, the better. That’s why it’s so important to tell a provider whenever you notice changes in your skin.
Advertisement
The overall 10-year survival rate for people with early-stage (Stage I or II) CTCL is 90%. That means that 9 out of 10 people with this condition are still alive 10 years later. People with late-stage CTCL (Stage III or IV) have an overall 10-year survival rate of 53%.
Survival rates are estimates. They can’t tell you how long you’ll live or how you’ll respond to treatment. To learn more about survival rates and what they mean for you, ask your healthcare provider.
Most people who have CTCL have no changeable risk factors. So, there’s nothing you can do to prevent it. But researchers continue to study why these conditions happen.
Even though you can’t prevent cutaneous T-cell lymphoma, a weakened immune system could make you more susceptible to CTCLs and all types of cancer. Here are some ideas for keeping your immune system strong:
Cutaneous T-cell lymphoma affects your skin, making it dry, itchy and scaly. While treatment slows cancer growth and eases symptoms, some treatments may irritate already aggravated skin. Here are some suggestions that may help:
Advertisement
Your healthcare provider will want to see you for regular checkups. Ask them how often you should see them for blood tests or skin exams.
Advertisement
Always contact your healthcare provider if you:
It’s normal to assume that symptoms like rash and discoloration point to common skin conditions. It’s hard to imagine that a rare cancer could be the culprit. But it’s important to let a healthcare provider know any time you notice skin changes. They can determine the cause. Maybe it’s not cancer. But if it is, treatment is key. The sooner you start it, the better your overall outlook.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you hear that you might have lymphoma, you want care from experts you can trust. At Cleveland Clinic, we craft a treatment plan tailored for you and your needs.
