Hyperaldosteronism happens when one or both of your adrenal glands produce too much aldosterone, a hormone. It causes high blood pressure and has several possible causes. Hyperaldosteronism is treatable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
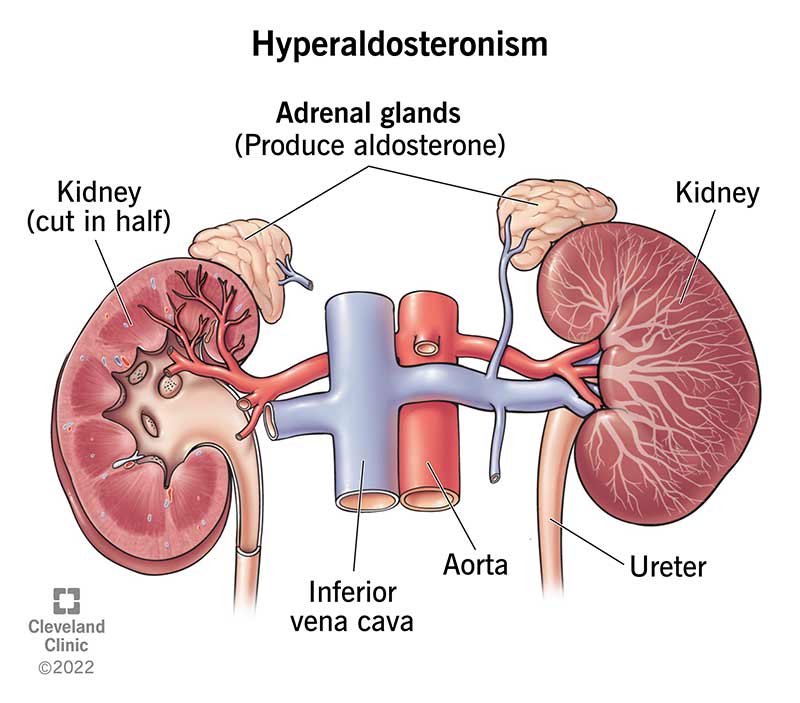
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16448-hyperaldosteronism-illustration)
Hyperaldosteronism is a condition in which one or both of your adrenal glands produce too much aldosterone. Aldosterone is a hormone that helps regulate your blood pressure by controlling the levels of potassium and sodium in your blood.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your adrenal glands are part of your endocrine system. They make hormones your body needs to carry out daily functions. You have two adrenal glands — one atop each kidney.
There are two main types of hyperaldosteronism:
Hyperaldosteronism causes high blood pressure (hypertension) and low potassium levels in your blood.
Hyperaldosteronism mostly affects people 30 to 50 years old. It more often affects women than men.
It’s difficult for researchers to estimate how common hyperaldosteronism is. Some studies suggest that 5% to 10% of people with high blood pressure have primary hyperaldosteronism. Experts estimate that as many as 25% of people who have medication-resistant high blood pressure may have hyperaldosteronism.
The symptoms of hyperaldosteronism can vary based on the severity of the condition. Some people with mild cases of hyperaldosteronism have no symptoms (are asymptomatic).
The most common symptom of hyperaldosteronism is high blood pressure (hypertension), especially medication-resistant hypertension.
Advertisement
If you experience other symptoms, they’ll probably be caused by having moderate to severe high blood pressure and/or low potassium levels (hypokalemia).
Symptoms of high blood pressure include:
Symptoms of low potassium include:
Hyperaldosteronism has different causes depending on the type: primary or secondary.
Primary hyperaldosteronism happens when there’s an issue within your adrenal glands that causes them to produce too much aldosterone.
Adrenal adenomas (noncancerous tumors) are the most common cause of primary hyperaldosteronism.
Rarer causes of primary hyperaldosteronism include:
Reduced blood flow to your kidneys causes secondary aldosteronism.
To understand why this happens, it’s important to know that aldosterone is part of a complex chain of hormone reactions that regulates your blood pressure.
This is known as the renin-angiotensin-aldosterone system, and it involves the following steps:
Reduced blood flow to your kidneys “mistakenly” triggers the renin-angiotensin-aldosterone system, which results in excess aldosterone in your body.
Causes of reduced kidney blood flow and secondary hyperaldosteronism include:
A healthcare provider will diagnose hyperaldosteronism with blood tests. However, many people never have hyperaldosteronism diagnosed because several conditions and risk factors can cause high blood pressure.
General signs of hyperaldosteronism include medication-resistant high blood pressure and the following results of an electrolyte blood panel:
Advertisement
If your healthcare provider thinks you might have hyperaldosteronism based on these signs and your symptoms, they’ll likely order one of two blood tests: plasma renin concentration (PRC) or plasma renin activity (PRA).
If you have primary hyperaldosteronism, your PRC and PRA levels will be lower than normal. In secondary hyperaldosteronism, the levels will be higher than normal.
You may also need an aldosterone suppression test. This test involves consuming a certain amount of sodium (salt) orally or through an IV over a certain amount of time. You’ll then provide urine (pee) samples over a 24-hour period so that a laboratory can measure the amount of aldosterone in your pee.
If these tests confirm you have hyperaldosteronism, your provider will order additional tests to determine the cause. For example, they may recommend an imaging test such as a CT (computed tomography) scan to check for a tumor that could be causing hyperaldosteronism.
The treatment of hyperaldosteronism depends on what’s causing it. But the main goal is to manage your blood pressure.
Healthcare providers usually recommend treating primary hyperaldosteronism caused by an adrenal gland tumor by surgically removing the tumor. In some cases, these tumors can be treated with only medication. Even after surgery, you might still have high blood pressure and need to take medicine to manage it.
Advertisement
Providers treat secondary hyperaldosteronism by managing your blood pressure with medications and treating the underlying cause (such as heart failure).
Medications that can help treat hyperaldosteronism include:
Men may experience erectile dysfunction and gynecomastia (enlarged male breast tissue) with long-term use of medicines that block the effects of aldosterone, such as spironolactone.
The prognosis of hyperaldosteronism varies depending on what caused it.
The outlook for primary hyperaldosteronism is generally good if it’s diagnosed and treated early. The outlook for secondary hyperaldosteronism depends on the cause of the condition.
The most common complications of hyperaldosteronism are cardiovascular issues caused by high blood pressure, including:
In most cases, there’s nothing you can do to prevent hyperaldosteronism.
If you’ve been diagnosed with hyperaldosteronism, you’ll need to see your healthcare provider regularly to make sure your medication dosage is working.
Visit a healthcare provider if you notice any new symptoms or if your symptoms are changing.
Advertisement
Hyperaldosteronism is one of the many causes of high blood pressure. The good news is that it’s treatable. If you’re experiencing high blood pressure that’s resistant to treatment, talk to a healthcare provider about the possibility of having hyperaldosteronism. They can recommend some tests to check your health.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your hormones are out of balance, so are you. Cleveland Clinic experts can diagnose and treat some adrenal disorders to help you feel like yourself again.
