Charcot foot is damage to your foot when you’ve lost feeling in your feet and ankles. You may not to notice or feel symptoms of an injury or infection that’s hurting your foot. The longer these issues are untreated, the more damage they can do. It’s important to see a healthcare provider for regular foot exams if you have diabetes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
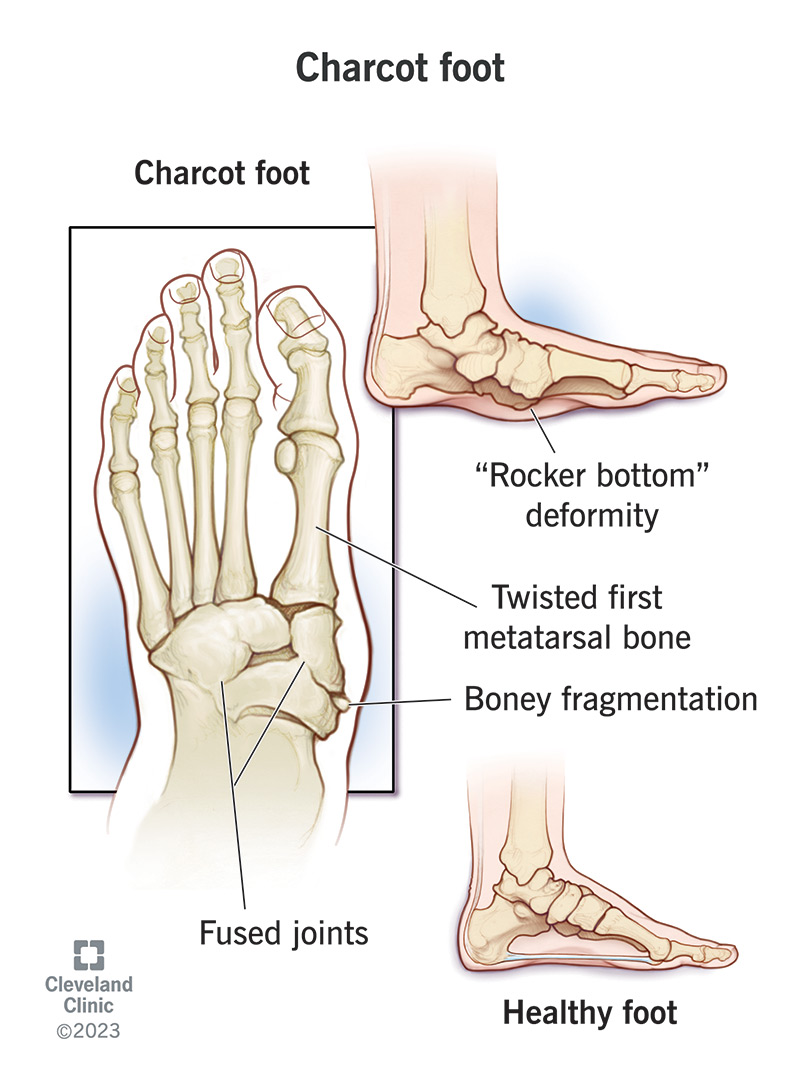
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15836-charcot-foot)
Charcot foot is a rare complication of diabetes-related neuropathy. It can make injuries or infections much more serious.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Diabetes-related neuropathy is nerve damage that makes you lose feeling in your lower legs and feet. This makes it hard (or impossible) to feel pain or notice other signs that something is hurting your foot. Charcot foot happens when a small injury or an infection causes severe complications because you can’t feel or notice the symptoms.
If it’s not treated soon enough, Charcot foot can make the joints in your foot collapse and permanently affect your ability to use your foot. It can also make it more likely that an infection in your foot gets much worse or spreads to the rest of your body. In severe cases, this can lead to needing your foot amputated or cause life-threatening complications.
Talk to a healthcare provider about managing diabetes and your blood sugar (blood glucose) levels. The best way to prevent Charcot foot is to have regular checkups with a provider and examine your feet for any loss or change in your ability to feel touch, pain or pressure.
Some other names healthcare providers use instead of Charcot foot include:
Charcot foot is rare. It affects less than 1% of all people with diabetes.
Early symptoms of Charcot foot include:
Advertisement
Visit a healthcare provider as soon as you notice any changes in your feet. The sooner your provider can diagnose Charcot foot, the less likely you’ll experience severe complications.
More advanced Charcot foot can cause changes to your foot’s shape (Charcot foot deformity), including:
Charcot foot happens when you injure your foot or get an infection but can’t feel symptoms like pain. It’s usually a diabetes-related foot condition:
For example, people with Charcot foot might not be able to feel the pain signaling that their bones, tendons or ligaments are damaged and keep walking on an injured foot. A usually minor ankle injury or a bone fracture can become much worse if you keep walking on your foot without feeling pain or knowing it’s hurt. Over time, that extra stress can cause permanent damage to the shape of your foot and ankle.
Similarly, if you have Charcot foot and can’t notice symptoms like pain or a feeling of warmth, you might miss symptoms of an infection until after it’s caused severe complications.
Advertisement
Charcot foot almost always affects people with diabetes. People who’ve had diabetes for more than seven years who smoke and regularly drink alcohol have an increased risk of developing neuropathy.
You’re also more likely to develop neuropathy if you have diabetes and have other health conditions, including:
Charcot foot itself is a complication of diabetes-related neuropathy. If your foot is damaged enough or you have a serious infection you might experience other severe complications, including:
A healthcare provider will diagnose Charcot foot with a physical exam and some imaging tests. Tell your provider if you’ve noticed any symptoms like pain, swelling, a feeling of warmth or if you’ve lost some feeling in your ankles, feet or toes.
Advertisement
Your provider will examine your ankles and feet. They’ll check both your feet and compare them to look for changes or differences. Your provider will also check how much feeling you have in your feet by touching your ankles, feet and toes.
Your provider might use a few tests to diagnose Charcot foot, including:
Preventing severe complications is the most important part of treating Charcot foot. You need to stop walking on your foot before any injuries or issues get worse (progress). Your healthcare provider will suggest treatments to relieve your symptoms and reduce how much Charcot foot permanently affects your ability to use your foot.
The most common treatments for Charcot foot include:
Putting less weight and pressure on your affected foot reduces swelling and prevents injuries like bone fractures from getting worse. You might need:
Orthotics are shoe inserts that support your feet and keep your toes in the correct position. You might need custom-made inserts or an ankle brace. Your provider will recommend orthotics or special shoes with extra depth to help relieve extra pressure on your feet and support you when you walk.
Advertisement
A physical therapist is a healthcare provider who helps you improve how your body performs physical movements. They’ll help you manage symptoms like pain, stiffness and discomfort that make it hard to move. They’ll also develop a customized set of exercises and movements to help you move your body.
You might need Charcot foot surgery if you’re experiencing severe symptoms (including collapsed bones and joints or ulcers) or have an infection that might spread.
Your surgeon will repair damage inside your foot and ankle joint and will stabilize your foot. It’s rare, but people with severe Charcot foot may need their foot amputated.
Your surgeon will tell you which procedure you’ll need and what to expect while you’re recovering.
If a healthcare provider diagnoses Charcot foot early, you should be able to avoid serious complications.
You’ll need regular follow-up appointments with your provider. They’ll take more X-rays to check your feet for any changes or new symptoms.
If Charcot foot causes severe symptoms or complications, you might need to learn to walk and move differently, or use mobility aids. Your provider will help you understand what to expect. They’ll guide you on your recovery journey and will be there to answer all your questions.
The best way to prevent Charcot foot is to manage diabetes and your overall health. Managing your blood sugar will prevent hyperglycemia and reduce your risk for neuropathy.
Ask your healthcare provider how often you should have your feet checked. Ask them if you should see a foot care specialist like a podiatrist or a foot and ankle orthopedist.
You can also reduce the risk of Charcot foot and other diabetes-related foot problems by:
Visit a healthcare provider as soon as you notice any new or worsening symptoms in your feet.
If you have diabetes, tell your healthcare provider right away if you notice:
You should be able to walk and move with early Charcot foot. But don’t force yourself to use your foot, especially if you notice swelling or discoloration. They can be signs that your foot is injured, even if you can’t feel it.
Stay active, but choose activities that are gentler on your feet, like swimming or biking. Ask your provider which activities are safest for you.
Charcot foot is a rare complication that happens when diabetes damages nerves in your lower legs and feet. The best way to prevent serious complications from Charcot foot is to get it diagnosed as soon as possible. Visit a healthcare provider for regular checkups and foot exams if you have diabetes. Your provider will monitor your feet for any changes that could mean you’re at risk.
Talk to your provider about managing diabetes. They’ll help suggest resources that help you manage your blood sugar to reduce the chances you experience diabetes-related neuropathy and Charcot foot.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Whether you’ve been living with diabetes for years or you’re newly diagnosed, you want experts you can trust. Our team at Cleveland Clinic is here to help.
