Achalasia (cardiospasm) is a rare condition that happens when food and liquid doesn’t move through your esophagus to your stomach. Achalasia symptoms include trouble swallowing, heartburn and chest pain. It may cause complications like aspiration pneumonia. Treatment includes surgery and non-surgical options like medication and Botox injections.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
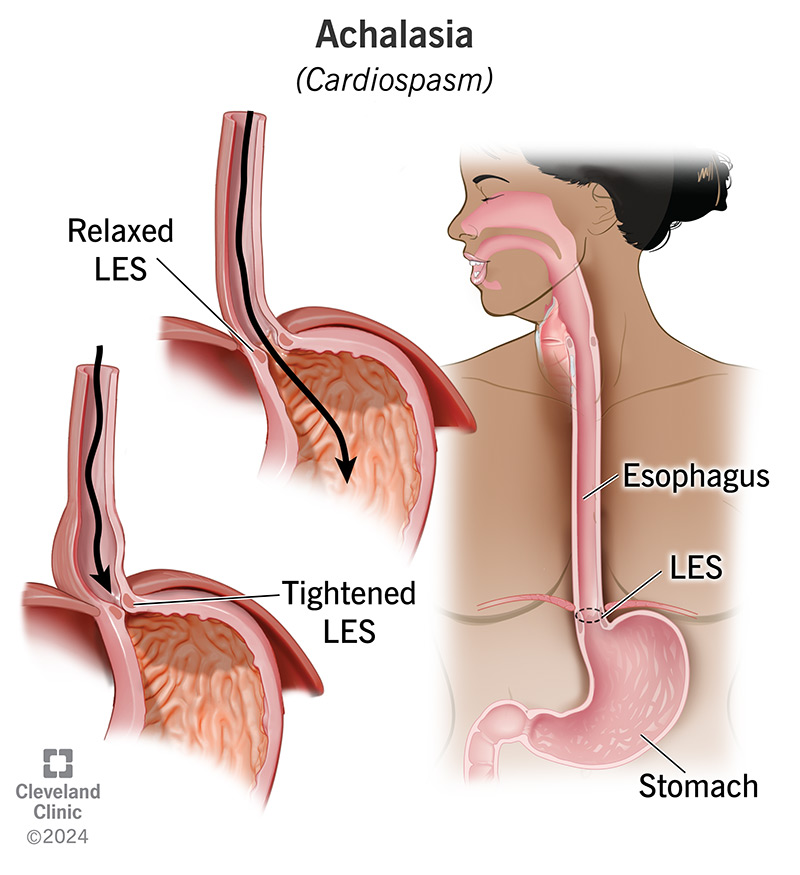
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/17534-achalasia.jpg)
Achalasia (ay·kuh·lay·zhuh) or cardiospasm is a rare esophageal disorder that develops when your esophagus doesn’t move food and liquid to your stomach like it should.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your esophagus is a muscular tube that runs from your mouth to your stomach. Normally, muscular contractions (peristalsis) in your esophagus push food and liquid down to your lower esophageal sphincter (LES). Your LES is a ring-shaped muscle that relaxes (opens) to let food move into your stomach and tightens (contracts) to keep contents in your stomach from backing up into your esophagus.
In achalasia, peristalsis doesn’t take place or doesn’t work as well as it should. And when it does, your LES doesn’t relax, so what you eat and drink stays in your esophagus instead of moving into your stomach. You have trouble swallowing your food or have other symptoms. You may lose a lot of weight and may develop malnutrition.
Cardiospasm affects 1 in 100,000 people in the U.S. It typically affects adults ages 25 to 60, but kids may develop it. Treatment includes surgery and medication, but achalasia symptoms often come back.
Cardiospasm symptoms develop slowly. You can have this disorder for months or years before noticing changes in your body. Symptoms include:
Advertisement
Experts don’t know the exact reason why your esophagus doesn’t work like it should. One theory is that achalasia is an autoimmune disease (your body attacks itself) that a virus triggers. In this theory:
If you have achalasia, food may back up into your esophagus and into your windpipe, so you inhale food into your lungs. If that happens, you may develop complications like:
A healthcare provider will do a physical exam. They’ll ask you to describe your symptoms and how long you’ve had them. Providers commonly use these three tests to diagnose cardiospasm:
Treatment focuses on relaxing your LES, the ring of muscle at the base of your esophagus. Treatment can’t cure achalasia, but nonsurgical and surgical options can help ease symptoms. Your healthcare provider will plan treatment depending on factors like your symptoms and your personal preferences. They’ll discuss these options with you so you both can decide what treatment makes sense for you.
Nonsurgical treatments for achalasia include balloon dilation and medication. Here’s more information:
Your provider may recommend one of two noninvasive surgeries to loosen your lower esophageal sphincter (LES). Those surgeries are:
Very rarely, your symptoms may be so severe that your provider will recommend an esophagectomy to remove your esophagus.
Advertisement
Research shows laparoscopic Heller myotomy and POEM surgery are effective, but may cause the following complications:
Achalasia symptoms often come back after treatment. You’ll need long-term follow-up so your healthcare provider can:
Without treatment, achalasia may lead to malnutrition, which can be life-threatening and affect your life expectancy. With treatment, you may expect to live as long as other people who don’t have the disorder.
Achalasia may come back after treatment. The disorder’s symptoms develop over time. Here are some suggestions for ways to keep food moving and limit the impact the disorder can have on your life:
Advertisement
Cardiospasm makes it hard for food to move through your esophagus, particularly food that may:
Contact your provider as soon as you notice changes in your body, like new difficulty swallowing, which may be new achalasia symptoms.
Achalasia is a rare disorder that causes a wide range of symptoms that develop over time. It may cause everything from heartburn to hiccups to having a hard time swallowing your food. It’s understandable if you don’t make the connection between your various symptoms, much less the connection between your symptoms and something going on in your esophagus.
But even seemingly unrelated symptoms that don’t go away are a reason to talk to a healthcare provider. There are several ways to treat achalasia, and your provider will explain each treatment and recommend the one that’s right for you.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Swallowing disorders (dysphagia) can affect how you eat and drink. Cleveland Clinic is here to help you manage your dysphagia and feel better.
