Radiation therapy for breast cancer kills cancerous cells in tumors. People who have breast cancer surgery often receive radiation therapy afterward to eliminate cancer cells that remain after surgery. Radiation therapy for breast cancer can cause short-term and long-term side effects.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
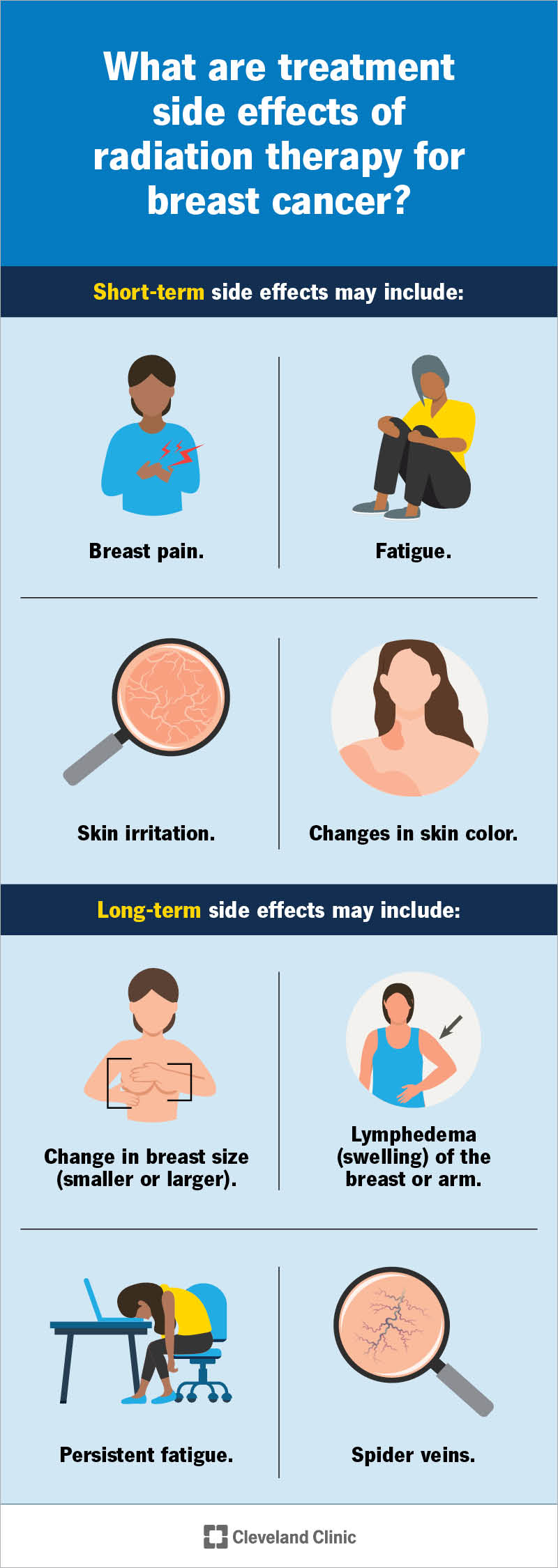
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/9191-radiation-therapy-breast-cancer)
Radiation therapy for breast cancer uses high-powered X-rays to kill or damage cancerous cells in your breast. Breast surgeons/surgical oncologists (cancer specialists) often do breast cancer surgery to remove tumors. Then, radiation oncologists oversee radiation therapy to eliminate remaining cancerous cells. People with metastatic breast cancer may have this treatment to ease breast cancer symptoms or symptoms from other areas of their bodies.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are different ways to receive radiation therapy. Your radiation oncologist will choose the best method based on the cancer location, type and other factors.
Types of radiation therapy for breast cancer include:
Your first appointment is a planning session and a chance for your radiation oncology team to explain processes and answer your questions. The team will:
Advertisement
Knowing what to expect may help you make plans and coordinate your personal activities like work and other obligations.
The planning session also involves a simulation. In simulations, your radiation oncology team uses a computed tomography (CT) scan to map out the area on your breast they need to treat. Simulation may take an hour or more.
During the simulation, a team member will:
When you arrive for treatment, a team member will greet you and give you a medical gown to wear during treatment. Next, they’ll:
Advertisement
Typically, radiation therapy doesn’t cause immediate side effects, but you may have short-term and long-term reactions.
Short-term side effects may include:
Long-term side effects may include:
Advertisement
Unlike some forms of chemotherapy, most people don’t lose their hair from their heads during radiation therapy, but they may lose armpit hair.
Radiation therapy is an effective way to target breast cancer tumors without damaging nearby tissues. Research shows breast cancer is less likely to come back (recur) in people with early-stage breast cancer who have radiation therapy after surgery. According to the American Society of Clinical Oncology, less than 5% of people have recurrent breast cancer 10 years after surgery and radiation therapy.
Rarely, radiation therapy for breast cancer causes complications, like issues that affect your chest. Potential complications include:
Radiation therapy can make your skin feel very tender, itchy and painful. It may affect your appetite and make you feel very tired. Here are some suggestions to help you through treatment:
Advertisement
That depends on your situation. You’ll probably feel OK when you first start treatment and then notice you have less energy and feel more tired as treatment continues.
Let your provider know anytime you have side effects that are more severe than you expected.
You may want to ask the following questions when you meet with your radiation therapy team:
Radiation therapy for breast cancer is a common, effective treatment for early-stage and more advanced breast cancer. It may also help ease symptoms of metastatic breast cancer. Studies show this treatment keeps breast cancer from coming back. The treatment may cause short-term and long-term side effects. If you have breast cancer, talk to your healthcare providers about radiation therapy. They’ll be glad to explain the treatment and how it may fit into your plan for conquering breast cancer.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic offers expert radiation oncology with advanced technology, personalized care and virtual visits to support you every step of the way.
