Hemorrhoids, or piles, are a common condition. These swollen veins inside of your rectum or outside of your anus can cause pain, anal itching and bleeding. Symptoms often improve with at-home treatments. Eating more fiber and avoiding straining can help prevent hemorrhoids.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
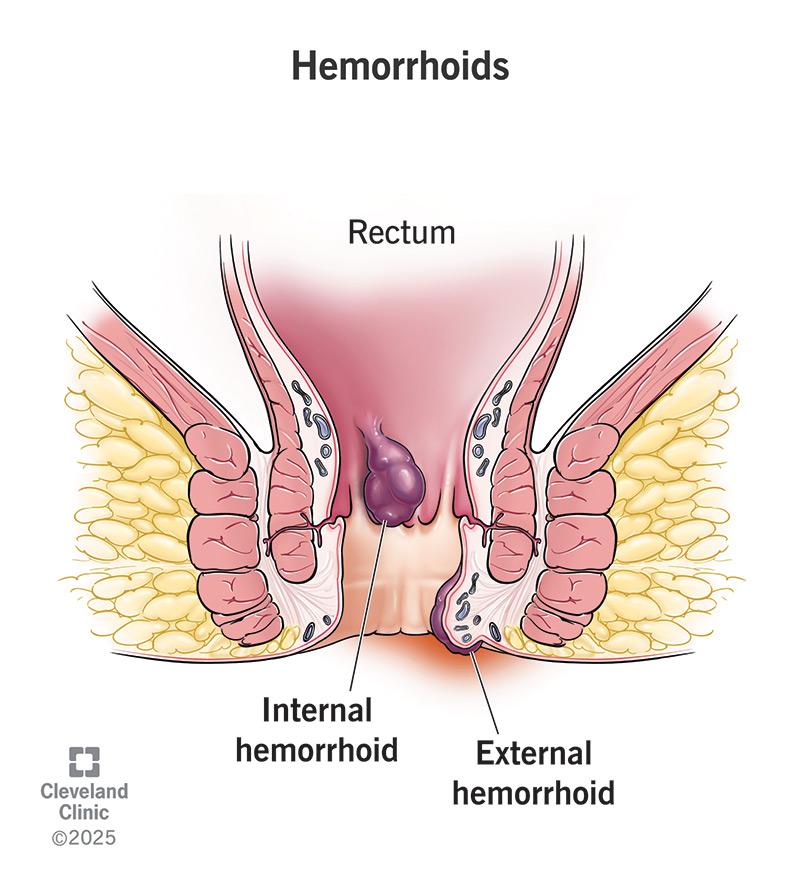
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/15120-hemorrhoids.jpg)
Hemorrhoids are swollen, enlarged veins that form inside and outside of your anus and rectum. They can be painful and uncomfortable and cause bleeding. Hemorrhoids are also called piles.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
We’re all born with hemorrhoids, but they typically don’t bother us. It’s only when they swell and enlarge that they produce irritating symptoms.
An estimated 1 in 20 Americans have hemorrhoids that are bothersome. They affect people of all ages, races and ethnicities. They’re more common as you age, affecting more than half of people over age 50.
Hemorrhoids can happen inside or outside of your rectum. The type depends on where the swollen vein develops. Types include:
Internal hemorrhoids rarely cause pain (and typically can’t be felt) unless they prolapse. Many people with internal hemorrhoids don’t know they have them because they’re inside your rectum. If you have symptoms of internal hemorrhoids, you might see bright red blood on toilet paper, in your poop or in the toilet. If an internal hemorrhoid prolapses through your anus, you may be able to gently push it back inside.
Advertisement
External hemorrhoids tend to be a little more noticeable because they happen outside your anus. Signs and symptoms of external hemorrhoids include:
A thrombosed hemorrhoid is when blood pools inside an external hemorrhoid. This can cause similar symptoms like swelling, inflammation and pain, but it’s typically much more severe and sudden.
Hemorrhoids look different depending on the type. You won’t see an internal hemorrhoid unless it protrudes (prolapses). A prolapsed internal hemorrhoid is usually a small lump around your butthole that you can push back in.
Non-thrombosed external hemorrhoids are usually the color of your skin. They’re soft to the touch and you can’t push them back in. Thrombosed external hemorrhoids may appear blue, black or purple and be firmer to touch. They’re often more painful.
Keep in mind that not all lumps are hemorrhoids. It’s important to contact a healthcare provider for a diagnosis.
Too much pressure on the veins in your anus or rectum, as well as irregular bowel movements, cause hemorrhoids. This pressure and irritation lead to swelling and inflammation of your veins.
Some activities or conditions that cause pressure and lead to (or worsen) hemorrhoids are:
Hemorrhoids can be uncomfortable and painful, but they don’t tend to cause serious problems. Rarely, people with hemorrhoids develop:
A healthcare provider diagnoses hemorrhoids based on symptoms and a physical exam. They may be able to see an external hemorrhoid or a prolapsed hemorrhoid just by looking. You may also have:
Advertisement
These tests may be uncomfortable, but they aren’t painful. They typically take place in your provider’s office. A sigmoidoscopy may take place at an outpatient center with or without (twilight) anesthesia. You go home the same day.
Smaller hemorrhoids often go away with eating more fiber and changes to your toilet habits. Symptoms like pain and bleeding may last one week or slightly longer. In the meantime, you can take these steps to help ease your symptoms:
You should see your healthcare provider if symptoms get worse or interfere with your daily life or sleep. Also, seek help if signs don’t improve after a week of at-home treatments. Your provider may treat hemorrhoids with:
Advertisement
Surgical treatments include:
Hemorrhoids are common and you can’t always prevent them. But these steps can help reduce your risk of hard stools and constipation that can lead to hemorrhoids:
Advertisement
Most hemorrhoid symptoms improve within a week with at-home treatments.
You should call your healthcare provider if you have hemorrhoids and experience:
Other gastrointestinal disorders can cause rectal bleeding and symptoms like hemorrhoids. Some of these disorders are life-threatening. For this reason, it’s important to let a healthcare provider know when you’re having symptoms.
You may want to ask your healthcare provider:
Hemorrhoids and anal fissures cause similar symptoms, such as itching, pain and bleeding. While swollen veins cause hemorrhoids, an anal fissure is a tear in the lining of your anus. Similar issues with irregular bowel movements and straining can cause both. A healthcare provider will do a physical exam and may order tests to find what’s causing your symptoms.
Millions of people seek treatment for hemorrhoids at some point in their lives. But many more never seek treatment and experience discomfort caused by hemorrhoids. Don’t let embarrassment or fear stop you from talking to a healthcare provider. You aren’t the first to talk to them about hemorrhoids, and you won’t be the last.
If hemorrhoids cause you pain or discomfort, a healthcare provider has treatments that can help. You can also take steps to keep hemorrhoids from coming back.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When hemorrhoids cause pain or bleeding, you want the best possible care. Cleveland Clinic’s providers can make you more comfortable with a variety of treatments.
