Glaucoma refers to many diseases involving eye pressure increases that lead to permanent vision loss and blindness. This condition can happen for many reasons, but most are treatable. Knowing the risk factors and getting regular eye exams may help you avoid vision loss.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_thjc82a4/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Mary Qiu, MD answers common questions about glaucoma.
Glaucoma is an umbrella term for eye diseases that make pressure build up inside your eyeball, which can damage delicate, critical parts at the back of your eye. Most of these diseases are progressive, which means they gradually get worse. As they do, they can eventually cause permanent vision loss and blindness. In fact, glaucoma is the second-leading cause of blindness worldwide.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Learning that you have glaucoma or that you’re at risk for it can be hard to process. For most people, vision is the sense they rely on most in their daily routine. It can feel scary to imagine trying to adapt to and live your life after you have severe vision loss. But most forms of glaucoma are treatable, especially when diagnosed early. And with care and careful management, it’s possible to delay — or even prevent — permanent vision loss.
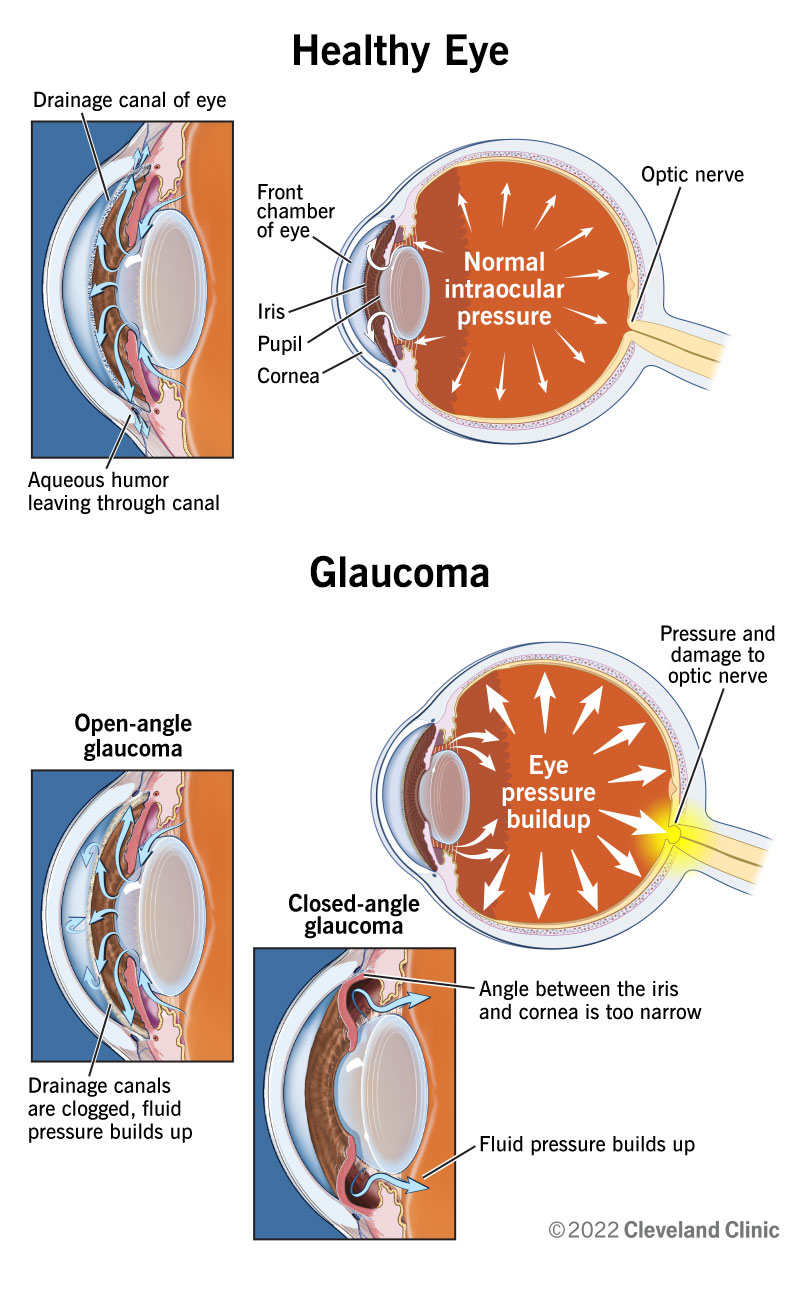
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4212-glaucoma.jpg)
In its early stages, glaucoma may not cause any symptoms. That’s why up to half of the people in the United States with glaucoma may not know they have it. And symptoms may not appear until this condition causes irreversible damage.
Some of the more common glaucoma symptoms include:
Some types of glaucoma, particularly angle closure glaucoma, can cause sudden, severe symptoms that need immediate medical attention to prevent permanent vision loss. Emergency glaucoma symptoms include:
Advertisement
Glaucoma is caused by damage to your optic nerve. It can occur without any cause, but many factors can affect the condition. The most important of these risk factors is intraocular eye pressure. Your eyes produce a fluid called aqueous humor that nourishes them. This liquid flows through your pupil to the front of your eye. In a healthy eye, the fluid drains through mesh-like canals (trabecular meshwork), which is where your iris and cornea come together at an angle.
With glaucoma, the resistance increases in your drainage canals. The fluid has nowhere to go, so it builds up in your eye. This excess fluid puts pressure on your eye. Eventually, this elevated eye pressure can damage your optic nerve and lead to glaucoma.
What makes the fluid build up can vary, depending on the specific overall type of glaucoma you have.
There are many different types of glaucoma, but they mainly fall under a few specific categories:
Several risk factors can contribute to glaucoma. They include:
Advertisement
Without care to manage it and lower the pressure inside your eye, glaucoma damages your retina and optic nerve to the point where they stop working. That causes glaucoma’s main complication: vision loss and, eventually, total blindness.
The end result is what experts call “absolute glaucoma.” That means you’re totally blind in the affected eye. The affected eye feels hard — and maybe even painful — when you touch it.
An eye care specialist can diagnose glaucoma using an eye exam, including several tests that are part of routine eye exams. In fact, eye exams can detect glaucoma long before you have eye damage and the symptoms that follow. Many of these tests involve pupil dilation (mydriasis), so your provider can get a better look inside your eye.
Some of the most helpful glaucoma tests include:
If your eye care specialist has a reason to suspect damage to your retina and/or optic nerve, they may also use additional types of eye imaging. These include:
Advertisement
The top priority for treating glaucoma is to keep it from getting worse by lowering the pressure inside your eye (intraocular pressure).
Some of the most likely treatments for this include:
Other treatments are possible, depending on what type of glaucoma you have, how it’s affecting your eye and other factors. Your eye care specialist can tell you more about your treatment options and help you choose one that fits your needs best.
Without treatment, glaucoma inevitably causes permanent vision loss and blindness. With treatment, it’s possible to slow the progress of the disease or stop it entirely. But because the range of possibilities can vary so widely, your eye specialist is the best person to talk to about this. They can tell you the likely outlook for your specific case and what you can do to help tilt the scales in your favor.
Advertisement
Glaucoma isn’t preventable, but early detection and treatment can manage pressure inside your eye and help prevent or delay vision loss. There are a few main ways that can happen:
If you have glaucoma, the best thing you can do is follow your eye care specialist’s guidance on treating and managing this condition. They may also recommend making certain changes to your life, habits or routine. These can include:
You should also see your provider if you notice new symptoms, if treatments aren’t as effective or if you have treatment side effects that are disrupting your life.
Angle-closure glaucoma usually develops quickly, so it needs immediate medical attention to prevent permanent damage and vision loss. The symptoms to watch for are the sudden onset or worsening of:
Some questions you may want to ask your eye care specialist include:
For most people, vision is an incredibly — if not the most — important sense. And the possibility of vision loss from a condition like glaucoma can make you feel anxious or afraid. Fortunately, glaucoma is a condition that’s detectable and treatable early. And the earlier you get a diagnosis and start treatment, the better the odds you can stop the disease from getting worse. Even if you can’t stop it, it’s usually possible to delay most cases of the disease so that the more severe effects don’t happen for years or even decades.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Glaucoma can cause vision loss if left untreated. Cleveland Clinic can quickly diagnose glaucoma and give you the ongoing expert treatment you need.
