Meningitis makes the protective layers surrounding your brain and spinal cord swell. Bacteria, viruses, fungi, parasites and noninfectious conditions can cause meningitis. Common symptoms include fever, neck stiffness and light sensitivity. If you think you have meningitis, go to the ER immediately.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
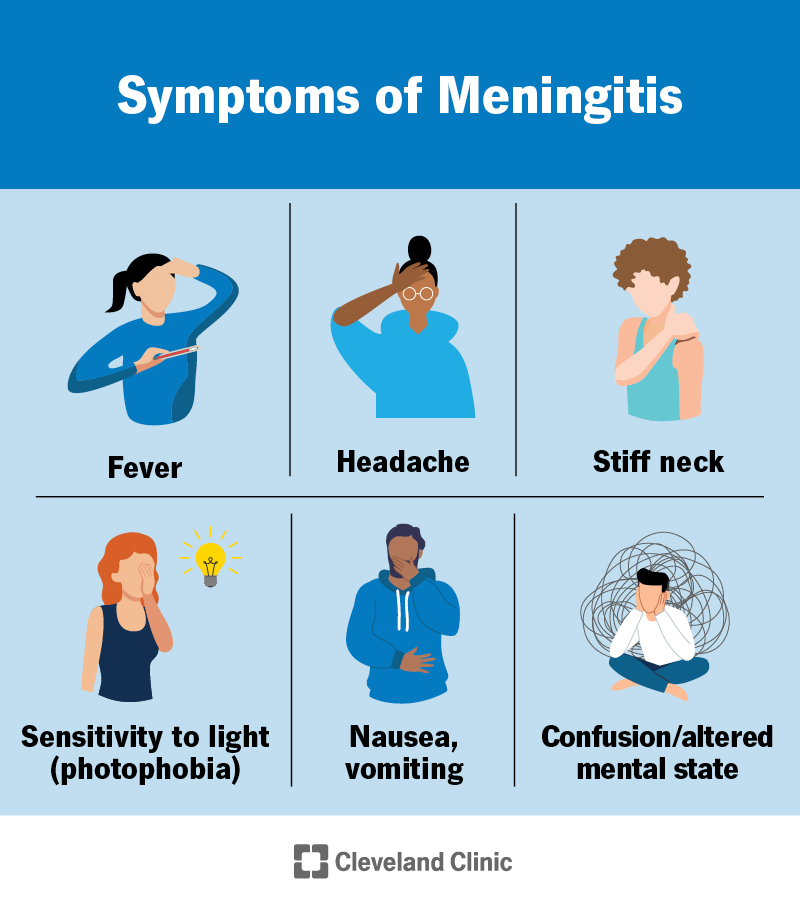
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/14600-meningitis)
Meningitis is inflammation of the three tissues that surround your brain and spinal cord, the meninges. Another name for it is spinal meningitis. This condition can be life-threatening.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your meninges normally protect your brain and spinal cord from injury. They contain nerves, blood vessels and cerebrospinal fluid (CSF). When your meninges become inflamed, they swell too much and put pressure on your brain and/or spinal cord.
Infectious diseases, like viruses and bacteria, can cause meningitis. Noninfectious conditions, like cancer and head injuries, can cause it, too.
Meningitis needs medical treatment right away.
Infectious types include:
Noninfectious types include:
Your healthcare provider may also describe meningitis as:
Symptoms of meningitis can vary depending on age.
Advertisement
Symptoms of meningitis in children and adults can include:
Signs of meningitis in babies can include:
If you have symptoms of meningitis, see a healthcare provider right away. A provider can diagnose it, find the cause and offer the best treatment.
Meningitis can cause severe headaches that can be quite painful. The pain may spread down your back or to other parts of your body. It may be almost impossible to move your neck in certain ways.
Some people have mild pain. Don’t wait for severe pain to see your healthcare provider if you have other symptoms of meningitis.
Infectious diseases (caused by something harmful from outside your body) and noninfectious conditions cause meningitis. Specific causes of each type include:
You can get meningitis in many ways, depending on whether the cause is infectious. You could get it:
Meningitis itself — swelling of the meninges — isn’t contagious. But some of its causes are. Most bacterial and viral causes of meningitis can spread from person to person.
Your age, where you live or travel, and certain health conditions can increase your risk of meningitis.
You’re at a higher risk for it if you:
Complications of meningitis can include:
Advertisement
Your healthcare provider will do a physical exam and ask about your symptoms. They’ll ask several questions about your medical history and recent activities, like whether you’ve traveled. This can help narrow down the cause of meningitis.
You’ll need tests to confirm the diagnosis and find the cause.
Some tests your healthcare provider may use to diagnose meningitis include:
Meningitis treatment depends on the cause. Medications treat most infectious cases. Treatment for noninfectious cases involves addressing the underlying condition or injury.
Medications and other therapies that may be a part of your treatment plan include:
Advertisement
Viral meningitis can go away on its own within about a week. Symptoms of bacterial or fungal meningitis may last a few days to a week or more after treatment. It can take weeks to months to feel completely recovered. Chronic meningitis may last for months to years.
Some people have long-lasting or permanent health issues from meningitis.
You’ll need follow-up appointments with your healthcare provider to make sure your treatment is working. It may be helpful to ask your provider these questions:
The outlook for meningitis depends on the cause, how severe it is and how soon you get treatment. With quick treatment, you can usually make a full recovery. But it can take a long time to feel completely well again.
You might have to stay in the hospital for a few days. Treatment may continue even after you go home. Your healthcare provider will follow up with you to check for lasting health concerns.
Yes, you can recover from most forms of meningitis. But it’s a very serious illness and requires immediate treatment.
Advertisement
Bacterial meningitis is the deadliest of the common forms of meningitis. According to the World Health Organization, about 1 in 6 people who get this type die. Around 1 in 5 has severe complications.
Meningitis isn’t always preventable. But there are steps you can take to reduce your risk of getting the infectious diseases that typically cause it. They include:
Your healthcare provider might also prescribe prophylactic antibiotics to help prevent a bacterial infection if you’re at high risk. Talk to your provider about prophylactic antibiotics if someone you live with or are around a lot has:
Meningitis is a serious condition that can have long-term consequences. Unlike injuries or illnesses that affect your body, you can’t see or feel your meninges beginning to heal. People may assume you’re completely recovered when you’re still working through issues, from hearing loss to thinking challenges. If that’s your situation, take the time to explain how meningitis continues to affect you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Have a virus, fungus or bacteria? Some of these “bugs” won’t go away on their own. Cleveland Clinic’s infectious disease experts are here to help.
