The stages of labor explain what you can expect to happen from the start of regular contractions through the delivery of the placenta. Healthcare providers use these stages to ensure your labor is progressing in a healthy way. Each labor experience is unique. But knowing what to expect in general can help you feel more prepared.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
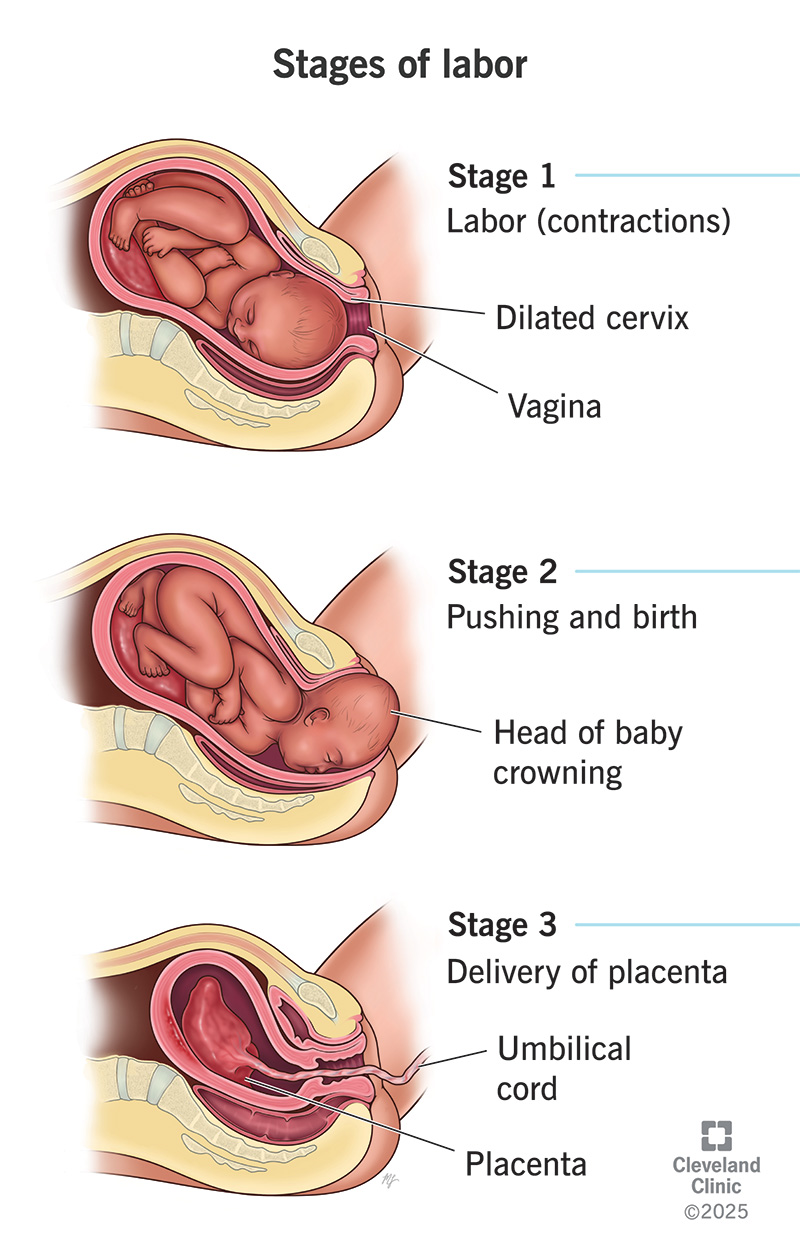
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22640-stages-of-labor)
The stages of labor are the process through which you deliver your baby and the placenta from your uterus through your vagina.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In general, the three stages of labor are:
Healthcare providers may call this “normal labor.” They use this definition and the stages to communicate effectively with each other and you. Just because you don’t go through every step of “normal” labor doesn’t mean there’s something wrong with your birthing experience.
You can experience some stages of labor, but your baby may arrive via C-section. Or you may never experience the first part of labor, like if you have a planned or emergency C-section. It may also be different if you have induced labor. Each labor experience is unique.
It can be stressful not knowing exactly what to expect for such a significant event. While pregnancy care providers know the general outline, they can’t predict how your labor will go. But rest assured that they’ll be by your side to guide you through the process. You have the shared goal of a healthy labor and delivery.
The first stage of labor begins with regular contractions. It ends with full dilation (opening) and effacement (thinning) of your cervix.
Most healthcare providers will ask that you time your contractions. When timing contractions, start counting from the beginning of one to the beginning of the next. It’s easiest to do this in seconds.
Advertisement
Regular contractions mean they’re strong and regularly spaced about three to five minutes apart. This is different from Braxton Hicks, which are irregular “practice” contractions. You may go into labor spontaneously or through medical induction in a hospital.
The first stage can last anywhere from 12 to 19 hours. If you’ve given birth before, you may go through this stage much faster.
This first stage has two phases:
Your pregnancy care provider will likely tell you that you can be at home for early labor. But you should be ready to go to your birthing center (like a hospital). During active labor, you should be at the birthing center.
During the first stage of labor, you may find it helpful to:
Having a labor support person is also very helpful. This could be your significant other, family member, friend or doula.
If it’s difficult to tolerate the pain, talk to your pregnancy care team about your labor pain relief options.
Everyone tolerates pain and discomfort differently. In general, it’s OK to sleep and rest during early labor if you’re able to. But you might find it difficult to sleep through the contractions.
The second stage of labor begins with complete cervical dilation (10 centimeters). It ends with the delivery of your baby. It can last anywhere from half an hour to several hours.
The fetus descends into your vagina with or without your pushing efforts. During the second stage of labor:
You may have your baby via a planned or unplanned C-section instead of vaginal delivery.
The third stage of labor begins with the delivery of your baby and ends with the delivery of the placenta. It’s the shortest stage and usually doesn’t last longer than 30 minutes.
Advertisement
During the third stage of labor:
If you have a C-section, your provider removes the placenta when they remove your baby from your uterus.
Your provider will make sure that all the placenta comes out. Retained products of conception can cause complications. If you had an episiotomy or vaginal tear, your provider repairs it once the placenta is out.
Scientists don’t know exactly how labor starts. But they think it results from a series of biochemical changes in your uterus and cervix. Both your body and the fetus have a role in these changes.
Your cervix has to go from firm and closed during pregnancy to thin and dilated. And your uterus has to start contracting (squeezing).
Experts believe that when the fetus is ready for birth, it releases a small amount of a substance that triggers your hormones to start the labor process. For most people, this happens naturally between 37 and 42 weeks of pregnancy. In some cases, a healthcare provider will induce (kickstart) labor.
Advertisement
Two main components of triggering and maintaining labor include:
Several pre-labor signs might hint that labor will start soon. These signs can include:
It can be difficult to know when you’re in true labor. If this is your first time, it can be easy to mistake other symptoms or irregular practice contractions (Braxton Hicks contractions) for true labor. True labor has a pattern and progresses steadily over time.
There are three things you’ll want to look for when you’re in true labor:
Advertisement
To protect the health of the fetus and you, healthcare providers follow guidelines that define abnormal labor. This is so they know when they may need to intervene to try to prevent complications. Before any sort of medical intervention, your care team will explain their concerns and the options.
Healthcare providers consider early labor to be prolonged if:
Providers consider active labor to be prolonged if:
Providers consider the second stage of labor to be prolonged if:
Providers consider the third stage to be abnormal if the placenta remains in your uterus more than 30 minutes after the delivery of your baby.
Ideally, you should be at your birthing center while you’re in active labor. This is the second phase of the first stage of labor.
Once your contractions are every five minutes for at least one hour, call your pregnancy care provider or the hospital labor floor. If your water breaks, whether or not you notice contractions, call your provider or the hospital labor floor. Even if it’s early in the first stage of labor, or if you think you’re having Braxton Hicks contractions, let your care team know what’s going on.
Get help right away if you experience:
When you get to the hospital, you’ll check in at the labor and delivery desk. You’ll probably go to a triage room first. This is part of the admission process. Hospitals usually recommend that you only bring one person with you to the triage room.
From the triage room, you’ll go to the labor, delivery and recovery (LDR) room:
The length of your hospital stay depends on the hospital and the type of delivery you have. Typically, you’ll stay in the hospital longer if you have a C-section because it’s a surgical procedure. You may also need to stay in the hospital for longer if you have any complications or health issues during your delivery.
Some experts consider the two to three hours after the delivery of the placenta to be a fourth stage of labor. This is the time when you may start to bond with your new baby. Your uterus also relaxes, and healthcare providers monitor you for any abnormal bleeding.
The average labor lasts 12 to 24 hours for a first birth and is typically shorter (eight to 10 hours) for subsequent births. The first stage of labor is usually the longest.
You’re bound to have a lot of feelings as you prepare for labor and delivery. It’s normal to feel both excited and nervous. Discussing the signs and symptoms with your healthcare provider can help you know what to expect. Your partner and healthcare team are there to support you. They’ll help you remain as comfortable and empowered as possible throughout the delivery process.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic childbirth experts coach you through every step — from labor to delivery to what to expect when you and your newborn head home.
