Alzheimer’s disease is a brain condition that slowly damages your memory, thinking, learning and organizing skills. It’s the most common cause of dementia. Symptoms usually first appear in people older than 65. There’s no cure, but medications may manage symptoms and slow its progression.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video playlist content: This video playlist is available to watch online.
View video playlist online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_i18c4vdo/flavorId/1_5f3sgelj/format/applehttp/protocol/https/a.mp4)
Learn more about living with Alzheimer's disease.
Alzheimer’s disease (AD) is the most common cause of dementia. Alzheimer’s is pronounced “alz-HAI-mers.” It’s a neurodegenerative disease that affects your brain. This means it damages and destroys cells in your brain over time. Eventually, people with AD lose some of their brain functions, including memory and language.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Alzheimer’s disease affects approximately 24 million people worldwide. One in 10 people older than 65 have it. Nearly 1 in 3 people older than 85 have AD.
Healthcare providers can suggest treatments to manage symptoms, but there’s no cure for Alzheimer’s disease. Talk to a provider if you’re worried you or a loved one have AD symptoms.
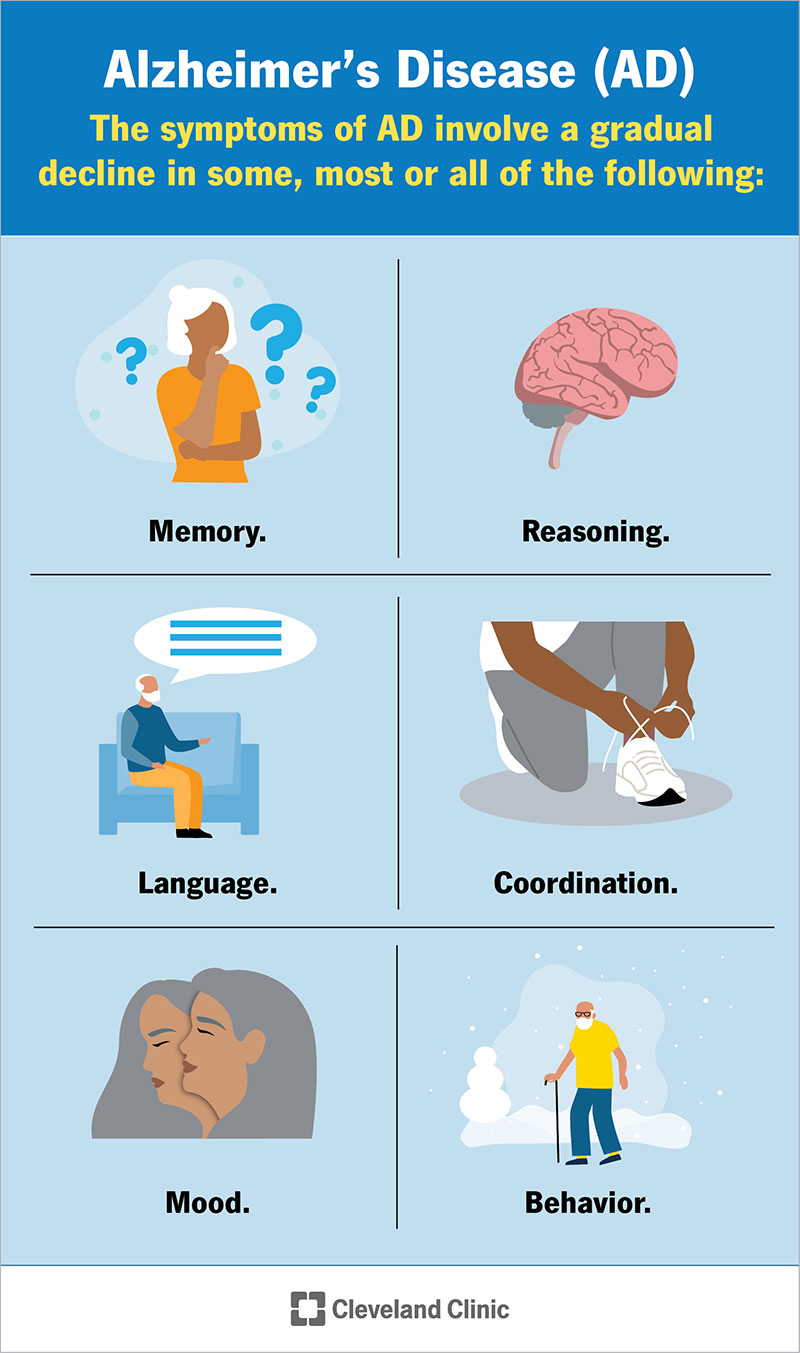
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9164-alzheimers-disease)
Alzheimer’s disease affects everyone differently. But in general, it can weaken or completely eliminate your:
People with memory loss or other Alzheimer’s symptoms may have difficulty recognizing changes in their own mind and body. These signs may be more obvious to loved ones.
Symptoms will get noticeably worse over time (a progressive decline). See a healthcare provider right away if you or a loved one have any dementia-like symptoms.
Memory loss is the most common Alzheimer’s symptom. It can affect your ability to recall recent events (short-term memory) or things that happened a long time ago (long-term memory).
You may have trouble remembering:
Memory issues from AD are different and more serious than occasionally forgetting where you left your phone or wondering if you locked the door when you came home.
Advertisement
Someone with Alzheimer’s might seem confused or like they’re taking an unusually long time to make a choice or decision. This can affect your ability to:
Alzheimer’s disease can make it hard for you to speak, read or understand language (aphasia). You may:
You might notice mood or personality changes in a person with Alzheimer’s disease. They might:
Everyone has a bad day or feels upset sometimes. But mood and personality changes caused by Alzheimer’s are more intense or sudden than everyday anger or grumpiness.
You may have a hard time understanding how close objects around you are from your body or feel less coordinated than usual. This can include:
Experts classify Alzheimer’s disease with stages. These stages can refer to how close you are to having dementia, the Alzheimer’s severity or how quickly it developed.
An abnormal build-up of proteins in your brain causes Alzheimer’s disease. Specifically, two proteins called amyloid and tau.
Your brain has billions of nerve cells called neurons. Your neurons let you think, learn, remember and plan. Amyloid protein sticks together in your brain cells, forming clumps called plaques. Tau proteins twist together in fiber-like strands called tangles. The plaques and tangles prevent neurons from working as they should. They block neurons’ ability to send electrical and chemical signals back and forth.
When amyloid and tau proteins build up in your brain, they slowly kill neurons. This causes permanent damage that leads to Alzheimer’s symptoms. Nerve cell death starts in one area of your brain and then spreads to other areas. It’s most common for Alzheimer’s to begin in the area of your brain that controls memory — your hippocampus.
Experts are still studying Alzheimer’s disease to learn more about what exactly causes these proteins to build up. Researchers think the protein build-up happens a long time before it causes symptoms. It might happen up to 10 years before you notice any changes.
Advertisement
Yes, Alzheimer’s can be hereditary (genetic).
Your risk of developing Alzheimer’s disease is 10% to 30% higher if you have a biological parent or sibling with it. You’re three times more likely than average to develop AD if two or more of your biological siblings have it.
Having the APOE ε4 gene increases your risk of developing Alzheimer’s. It’s also associated with developing AD at a younger age (an earlier age of onset). But not everyone who has the APOE ε4 gene will get Alzheimer’s. It’s just one factor that can increase your risk.
Researchers don’t know why some people get Alzheimer’s disease and others don’t. Some risk factors may include:
Some health conditions may increase your Alzheimer’s risk, including:
The biggest complication of Alzheimer’s disease is the damage it does to your brain. That can cause permanent changes to your ability to think, to use your body and to your personality. As the condition progresses, you’re likely to experience complications, some of which can be fatal.
Advertisement
Complications can include:
You may lose your ability to control your body. This can increase your risk of:
Healthcare providers diagnose Alzheimer’s disease in a few ways. The first step is discussing your current health and medical history.
Your provider will talk to you and your loved ones. They’ll ask you questions to understand your health and daily routine. Tell your provider if you know you have any risk factors for Alzheimer’s disease.
Your provider will ask your loved ones if they’ve noticed any symptoms or changes you might not be able to see in yourself. They might ask about your:
Your provider will also give you a complete physical exam and neurological exam. They’ll rule out other conditions that cause similar memory issues and other symptoms.
Advertisement
Your provider will also use a few tests, including:
These tests can help your provider look for signs of amyloid proteins and see if they have damaged your brain.
Your provider will work with you and your loved ones to develop a treatment plan that fits your unique needs. They’ll help you set realistic goals for your short-term health and long-term outlook.
Your provider will suggest treatments to slow down how fast you develop dementia. There’s no cure for Alzheimer’s, but treatments may manage symptoms as they happen and slow down the condition’s progression.
Starting treatment as soon as possible is the best way to maintain your brain health throughout your life. But there currently isn’t a treatment available that stops or reverses Alzheimer’s disease.
There are many medications that can manage Alzheimer’s symptoms. Your provider will suggest a combination that fits your unique needs. You might need:
These medications block an enzyme that can speed up how quickly Alzheimer’s damages your brain. They can improve some memory problems and reduce your risk of behavior changes. Your provider might prescribe:
Scientists are always researching Alzheimer’s disease and possible treatments. Ask your provider if there are any clinical trials that could help you. Clinical trials are tests or research studies done using human volunteers who have a condition or issue. A trial might help you try new treatments that aren’t widely available yet.
There may be more opportunities to participate in clinical trials the sooner you’re diagnosed.
Lecanemab and donanemab are intravenous (IV) infusions. They’re two types of monoclonal antibodies. These are medications that can help your body’s immune system target and destroy amyloid proteins. They can slow down Alzheimer’s progression by getting rid of some of the amyloid before it damages your brain.
Lecanemab targets amyloid fibers before they stick together. Donanemab targets amyloid proteins that have already clumped together to form plaques.
Like all other treatments, these medications aren’t cures for Alzheimer’s disease. And they can’t reverse any damage that amyloid has already done.
If you have Alzheimer’s, your body makes too much glutamate, which damages your brain’s cells. NMDA antagonists block or fill up the N-methyl-D-aspartate (NMDA) receptors glutamate binds to in your brain. This can slow down how fast Alzheimer’s progresses.
Memantine is a common NMDA antagonist. Your provider may suggest others depending on your health and which stage of Alzheimer’s disease you have.
Your provider will suggest medications or other treatments to manage specific symptoms as they develop. You may need:
Alzheimer’s disease affects everyone differently. Most people older than 65 with Alzheimer’s die within four to eight years of being diagnosed. But some people live for decades, especially if they were diagnosed before turning 65.
Talk to your provider about living with AD. They’ll help you set realistic goals and expectations. They can also help you and your loved ones decide when hospice care is a good option for you.
Talk to a mental health professional if you need support. It’s extremely common for people with AD and their loved ones to feel extra stress and anxiety, especially right after diagnosis. Those feelings are real and valid. A mental healthcare provider can help you process your thoughts and emotions.
There are some Alzheimer’s risk factors you can’t change or control, like your age and genetics. But you may be able to manage other factors to help reduce your risk. Maintaining your overall health can help protect your brain from cognitive decline. You can try to:
Talk to your provider about genetic testing if you’re worried about Alzheimer’s running in your biological family. They can screen you for the genes or genetic changes that may increase your risk of AD.
See a healthcare provider if you or a loved one are experiencing issues with memory or thinking. They can determine if the issues are due to Alzheimer’s or another condition.
You’ll need regular check-ups with your healthcare provider after you’ve been diagnosed with AD. Your provider will monitor the condition’s progression and adjust your treatments as needed.
You might want to ask your provider a few questions, like:
Alzheimer’s disease (AD) can be scary. It can feel like time has stopped or is moving too fast all at the same time. There’s no right or wrong way to live with a condition like Alzheimer’s disease.
Whether you have Alzheimer’s or are caring for a loved one living with AD, your healthcare providers are there for you. They’ll of course suggest treatments and clinical trials. But they can also answer your questions, connect you with resources and help make sure you understand what to expect.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Getting an Alzheimer’s disease diagnosis can be overwhelming. Cleveland Clinic offers the latest treatments, education and caring support for you and your family.
