A splenectomy is surgery to remove your spleen — the fist-sized organ that helps fight infection. You may need this surgery if you have a ruptured spleen, a blood disorder or cancer affecting your liver. You can live a normal lifespan without a spleen, but you’ll need to take precautions to prevent infections, like staying up to date on vaccines.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
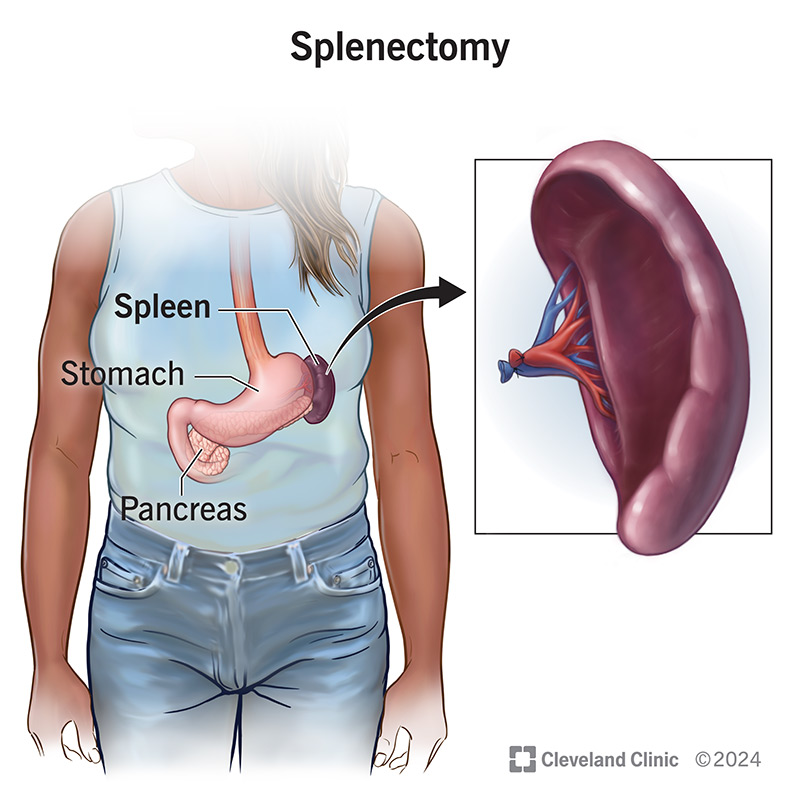
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/14614-splenectomy.jpg)
A splenectomy is surgery to remove your spleen. Your spleen is a fist-sized organ located in the upper left side of your abdomen. An important part of your lymphatic system (which makes up your immune system), your spleen makes white blood cells that help fight infections. It also filters old and damaged blood cells.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
An injury or disease that prevents your spleen from performing these functions may pose a threat to your health. In that case, you may need a splenectomy.
You can live without a spleen. In its absence, your liver and bone marrow take over most of your spleen’s functions. Still, your spleen is an important infection-fighter. Without it, you’ll need to take extra precautions, like getting regular vaccines, to prevent infections.
A splenectomy is a major surgery that removes an important organ. Your healthcare provider won’t recommend or perform a splenectomy unless it’s a medical emergency or other nonsurgical treatments haven’t worked.
But a spleen isn’t essential. You can continue to live a normal, healthy life (with a regular lifespan) without a spleen.
The most common reasons for a splenectomy include trauma (injury) to your spleen and treatment for a blood disorder.
Conditions that may require a splenectomy include:
Advertisement
Splenectomies are either medical emergencies or elective procedures (ones you can schedule ahead of time). If you’re having an elective splenectomy, preparation may involve:
Follow your provider’s guidance on if you need to fast or stop taking certain medicines, like blood thinners, before surgery.
Your surgeon can remove your spleen using one of two procedures: laparoscopy or open surgery. For both procedures, you’ll receive general anesthesia, so you’ll be asleep.
In most cases, your provider can perform a splenectomy laparoscopically. Laparoscopic surgery is minimally invasive. It requires smaller cuts than traditional open surgery, which makes for a faster recovery than open surgery.
During laparoscopy, your surgeon will:
Afterward, your surgeon will use stitches, staples or surgical glue to seal the wound.
You may need open surgery if your spleen is too large to remove with laparoscopy. Your surgeon may also use an open approach if you have out-of-control bleeding. It’s always possible that a laparoscopy may need to be converted to open surgery if there’s an issue.
The steps for an open surgery are similar to laparoscopy. The biggest difference is that instead of operating through a few small incisions, your surgeon operates through a larger single abdominal incision.
Advertisement
Once you’re able to tolerate a regular diet, move around without difficulty and your pain is under control, you’ll be discharged home. This usually occurs within two to three days with the laparoscopic technique and five to seven days with an open incision.
Before you’re discharged, your care team will ensure you understand how to navigate life without a spleen. This includes:
Advertisement
Getting vaccinated or continuing a vaccination series is one of the most important things you’ll do after a splenectomy. You’ll need:
Your vaccination schedule depends on your previous vaccination history and other treatments (for example, if you’re receiving chemotherapy). Generally, the vaccine schedule looks like this:
Possible complications include the usual risks of all surgeries, including bleeding, infection, injury to the surrounding abdominal organs and an allergic reaction to anesthesia.
A splenectomy increases your risk of blood clots and infections, including potentially fatal ones. Even minor infections can progress fast and become serious without a spleen. For example, a case of severe sepsis called overwhelming post-splenectomy infection (OPSI) can be fatal without treatment.
Advertisement
It’s essential to follow your healthcare provider’s recommendations to prevent infections and get treatment immediately if you’re experiencing symptoms. Acting fast can save your life.
The recovery period can take a few weeks up to six weeks. People heal more quickly after laparoscopy (as opposed to open surgery).
You can live a normal life expectancy after a splenectomy if you take precautions to prevent infection. Still, you’re two to three times more likely to get an infection or have a related complication (including death) if you’re living without a spleen.
This is why it’s so important to stay on top of all vaccines and follow your healthcare provider’s guidance to protect yourself.
Before discharge, talk to your provider about what symptoms or scenarios warrant a visit to the ER and which ones require a call to your healthcare provider. Be sure you understand before leaving.
Set up an appointment with your provider if you’re traveling, so you’re taking all necessary precautions to prevent infection.
Go to the ER if you’re experiencing signs of an infection, including:
Visit the ER if you’re bitten by an animal. These bites can lead to dangerous infections if you’re without a spleen.
A splenectomy is a major surgery that requires taking extra precautions moving forward to prevent infections. But a splenectomy doesn’t have to reduce your lifespan or quality of life. You can protect yourself by staying up to date on vaccines and acting fast at the first sign of an infection. Your healthcare provider can guide you on what steps to take to navigate life without a spleen.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Sometimes you have surgery planned. Other times, it’s an emergency. No matter how you end up in the OR, Cleveland Clinic’s general surgery team is here for you.
