A pneumothorax is when air gets inside your chest cavity and creates pressure against your lung, causing it to collapse partially or fully. Underlying medical conditions, injuries or medical procedures can cause it. Go to the nearest emergency department if you have symptoms of a pneumothorax, including difficulty breathing, chest pain or blue skin, nails or lips.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
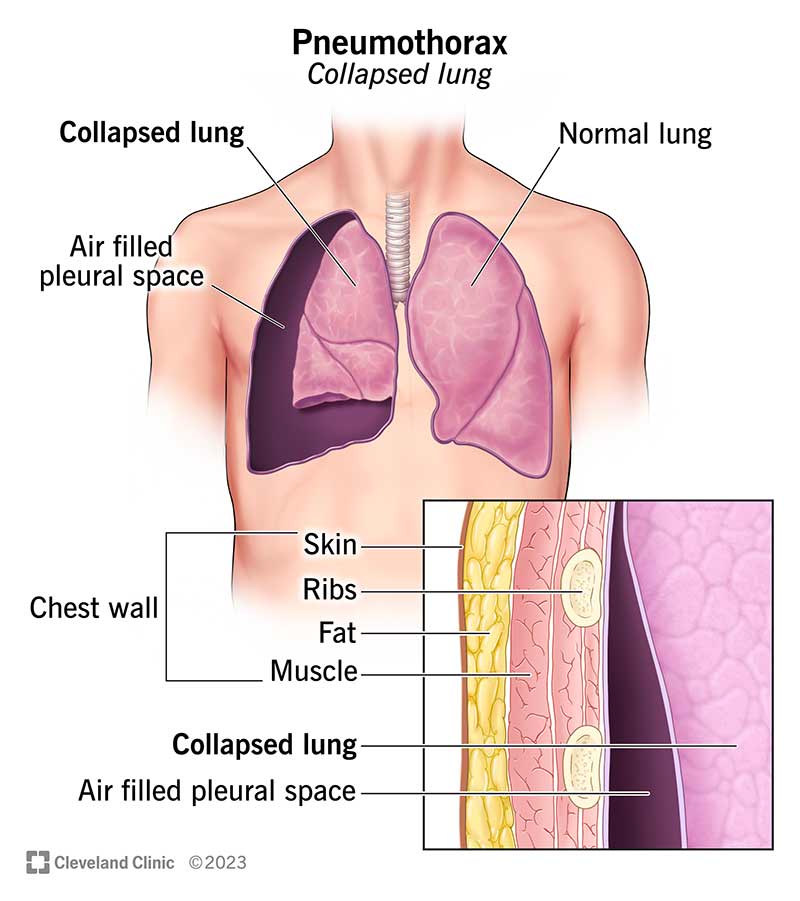
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15304-pneumothorax-illustration)
A pneumothorax (collapsed lung) happens when there’s air in the space between your chest wall and your lung (pleural space). Air in the pleural space can build up and press against your lung, causing it to partially or fully collapse. Pneumothorax is also called a punctured lung.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A pneumothorax can be a medical emergency. Go to the nearest emergency department right away if you think you could have collapsed lung.
The two main types of pneumothorax are spontaneous and traumatic.
A spontaneous pneumothorax is a collapsed lung that happens without an injury. Types include:
Injuries and medical procedures can cause a traumatic pneumothorax. Types include:
Other types of pneumothorax include:
Advertisement
The seriousness of a punctured lung depends on the cause and how much of your lung is collapsed. Some cases aren’t serious, and some are medical emergencies. A healthcare provider can tell you how much of your lung is collapsed and what your treatment options are.
Signs and symptoms of a pneumothorax include:
If you have symptoms of a collapsed lung, go to the nearest emergency room. You may need immediate care.
Pneumothorax has three main causes: medical conditions, injuries and lifestyle factors.
You might be more at risk for a collapsed lung if you:
Although most collapsed lungs heal without issues, some people have serious complications. These can include:
Providers usually diagnose a collapsed lung by listening to your lungs and by using imaging. This includes chest X-rays, CT scans (computed tomography scans) or a lung ultrasound. They may also use an arterial blood gas test to measure the levels of oxygen and carbon dioxide in your blood.
Your healthcare provider will ask about your history of lung disease and perform a physical exam. Some types of pneumothorax, like a tension pneumothorax, are diagnosed based on symptoms.
Your treatment depends on the cause, size and severity of your pneumothorax. Treatment may include:
Advertisement
Some people need surgery to repair damage so a punctured lung can heal. You may need surgery if you don’t respond to other treatments or have:
If you have a collapsed lung, you may be in the hospital for a couple of days or longer for treatment and monitoring. This allows your provider to check your progress and give you oxygen, if necessary.
Most of the time, a punctured lung can heal in a few days to two weeks. Your body reabsorbs the extra air around your lung, and your lung can reinflate.
Most people who have a punctured lung heal without major treatment. But you do have a chance that it’ll happen again (recurrence). Talk to your provider about your chances of recurrence and what to do if your symptoms come back.
Some cases of pneumothorax are life-threating. A collapsed lung should always be monitored by a healthcare provider.
To reduce your chances of a collapsed lung:
Advertisement
If you have certain medical conditions or a family history of pneumothorax, you might not be able to prevent a collapsed lung.
After going home from the hospital, it’s important to follow your provider’s recommendations for taking care of yourself. They may recommend you rest and limit or avoid certain activities, including:
Keep all your follow-up appointments with your provider after you go home.
Contact your provider if your symptoms return or get worse. If you’ve had a pneumothorax before, you might be at risk for it happening again.
Go to the emergency room if you have symptoms of a collapsed lung. You may need immediate treatment.
It might be helpful to ask your provider:
Many times, a pneumothorax can heal with minimal treatment. But any collapsed lung should be treated as a medical emergency until you know more. If you have signs or symptoms of a collapsed lung, such as chest pain or trouble breathing, get medical care right away. Your provider can determine the best form of treatment for you.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Breathing issues can affect your life in many ways. Cleveland Clinic’s respiratory therapy program treats your symptoms so you can feel better day to day.
