Intussusception is a medical emergency and form of bowel obstruction in which one segment of intestine telescopes inside of another. Although it can affect anyone, it’s most common in children between 3 months and 3 years old. A liquid contrast or air enema usually fixes intussusception. If it doesn’t, your child may need surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
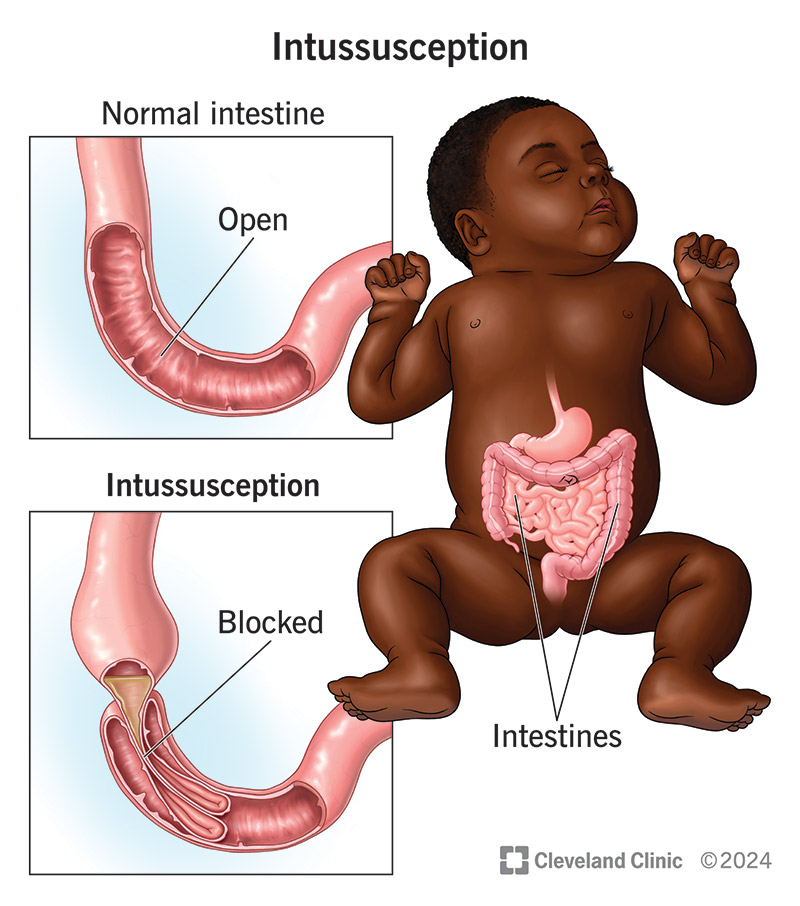
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/10793-intussusception.jpg)
Intussusception (pronounced “in-tuh-sus-SEP-shun”) is a medical emergency where one segment of your intestine folds partially inside the other, causing a bowel obstruction (blockage). Sometimes, the folding is described as “telescoping” because it resembles how the pieces fit into each other on a telescope. Usually, intussusception affects the small intestine (bowel).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Without treatment, the blockage can slow blood flow to your intestine and prevent food from passing through it. The obstruction can cause swelling and inflammation that leads to life-threatening complications.
Intussusception requires emergency care — but it’s treatable if you get help fast.
Anyone can develop intussusception, including adults, but it’s most common among children between 3 months and 3 years old.
Only 1% of adult bowel obstructions are related to intussusception. But intussusception is the most common reason children under 3 years old develop a bowel obstruction. Approximately 1 in 2,000 babies in the U.S. develop intussusception in their first year.
It’s important to recognize the signs of intussusception in your child and to be mindful of symptoms in the rare case that you develop this condition.
Babies and children with intussusception experience alternating episodes of severe, crampy abdominal (belly) pain followed by periods with no pain. The pain may last 15 to 20 minutes or longer. Children unable to communicate that they’re hurting may draw their knees up to their chests and cry. Then, they may appear fine and even start playing during the period of no pain (20 to 30 minutes) before the pain starts all over again.
Advertisement
Eventually, the cycle may exhaust your child, causing them to become lethargic (tired and slow-moving). They may develop a fever and go into shock.
Other possible symptoms of intussusception include:
Often, symptoms arise a few weeks or months after your child has been sick with a virus, so the timing of your child’s symptoms can raise your suspicion of intussusception.
Still, identifying signs of intussusception in your child can be challenging because it doesn’t always cause every symptom. The timing doesn’t always coincide with your child being sick.
Here’s a good rule of thumb: if your baby or small child appears to be experiencing unexplained belly pain, get them checked immediately.
Adults with intussusception also experience abdominal pain, but the pain may come and go (as in children) or remain constant. Vomiting, bloating and bloody stools are common, too. But, these symptoms are so common across various gastrointestinal (GI) conditions that many people wait things out. This is never a good idea with intussusception, though. It’s as much of a medical emergency with adults as it is with children.
In most cases of intussusception, healthcare providers aren’t sure of the cause.
In children, there does seem to be a relationship between viral infections and developing this condition. Most children develop intussusception in the fall and winter, the same time that the stomach flu (viral gastroenteritis) tends to spread. Other causes include irregular structures or growths in your child’s intestines, including Meckel’s diverticulum and polyps.
Causes in adults are more clear-cut. Adults with intussusception are more likely to develop it because they have colon cancer (malignant tumors) or benign (noncancerous) colon growths. Less commonly, intussusception can occur due to the long-term effects of inflammation (as with Crohn’s disease).
Risk factors include:
Certain conditions increase your child’s risk:
Advertisement
Conditions that increase your risk as an adult include:
Prompt treatment can typically fix the telescoping intestine. But, untreated intussusception can lead to life-threatening complications, including death. Complications include:
These complications can unfold quickly as your child’s condition worsens. This is why seeking emergency care is crucial if you suspect something’s wrong.
Diagnosis typically happens alongside emergency medical treatment. Imaging tests that confirm a diagnosis include an ultrasound (in children) and a CT scan (in adults). An ultrasound can identify an intussusception with 100% accuracy. It’s the first test providers use to check for an intussusception in children.
Advertisement
Your child’s provider may also order an air or contrast enema. During this test, your child’s provider inserts air or a liquid solution containing a safe substance called barium into your child’s rectum. The air or liquid creates pressure that helps lengthen the telescoped intestine so that one portion no longer folds inside the other. An X-ray records a video of the process.
In addition to confirming the diagnosis, this procedure usually fixes intussusception in children.
Treatment involves using an air or contrast enema (the same procedure used for diagnosis) to straighten out the telescoping in your child’s intestine. This is a radiologic (imaging) procedure, not a surgical one, so your child won’t need anesthesia.
This procedure isn’t effective in adults with intussusception, who usually need surgery.
Adults with intussusception need surgery, and (less often) so do some children. For example, if the enema doesn’t work or your child has a complication (like a bowel tear or an infection), they’ll need surgery.
The procedure may be a traditional “open” surgery, which involves one large cut in the abdomen. Or, the surgeon may use a less invasive procedure called laparoscopy.
During a laparoscopy, a surgeon makes two or three small incisions (cuts) into your child’s abdomen. These cuts allow a surgeon to access the telescoped intestine and position it into place. If repositioning isn’t possible, they’ll remove the involved segment of intestine and suture the remaining (non-telescoped) parts together.
Advertisement
A pediatric anesthesiologist (a specialist in pain relief in children) will sedate your child for the procedure so they don’t feel any pain and aren’t aware of what’s happening.
Your child may be gassy for a few hours after enema treatment. They may need acetaminophen (Tylenol®) to help with pain and manage fever.
After surgery, your child will need pain medicines to keep them comfortable. They’ll need to receive nutrition through IV fluids for several days while their intestines heal. Usually, they can begin eating again in one to three days. It may take a few weeks for them to return to their typical activity levels.
The prognosis is excellent for children treated early. An air or contrast enema usually cures intussusception. Intussusception recurs in 10% to 20% of children, with symptoms returning within the first 48 hours after surgery (less common) or weeks or months later (more common).
If intussusception returns, your child’s provider will take the same steps toward diagnosing and treating it. This may include doing another enema.
Ask your healthcare provider what to expect (including signs of a recurrence) before you leave the hospital.
A barium or air enema is successful in up to 85% of children treated in hospitals where providers have experience treating intussusception. You can improve your child’s chances of survival (with no complications) by getting them diagnosed and treated as soon as you notice symptoms.
There’s no way to prevent intussusception. But, you can take steps to avoid the worst outcomes by getting your child emergency treatment immediately.
Yes. An intussusception is always a medical emergency where time is of the essence. If your child shows signs of an intussusception, get them to a hospital that day as soon as possible.
If your child has unexplained belly pain, call their pediatrician immediately so they can be checked. If they can’t see you that day, get them to an emergency room (ER).
After treatment, you may notice some swelling around your child’s incisions. This is normal. However, call your child’s provider if your child develops:
Questions include:
Don’t second guess your concerns if you notice signs of intussusception in your baby or small child. A child that seems to be cycling through episodes of belly pain and then no pain is never normal. This may signal a serious condition, like intussusception. The sooner your child gets treated, the better their chance of survival with no complications. Don’t delay. Get them to their provider or the emergency room.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Whether you need stitches, a broken bone set or think your appendix might be causing your abdominal pain, Cleveland Clinic’s emergency medicine team is here to help.
