Ankylosing spondylitis (AS) is a type of arthritis that affects the joints in your spine. It usually develops in your sacroiliac joints (where the bottom of your spine joins your pelvis). It causes typical arthritis symptoms like pain and stiffness, but it can also cause digestive symptoms, rashes and weight loss.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
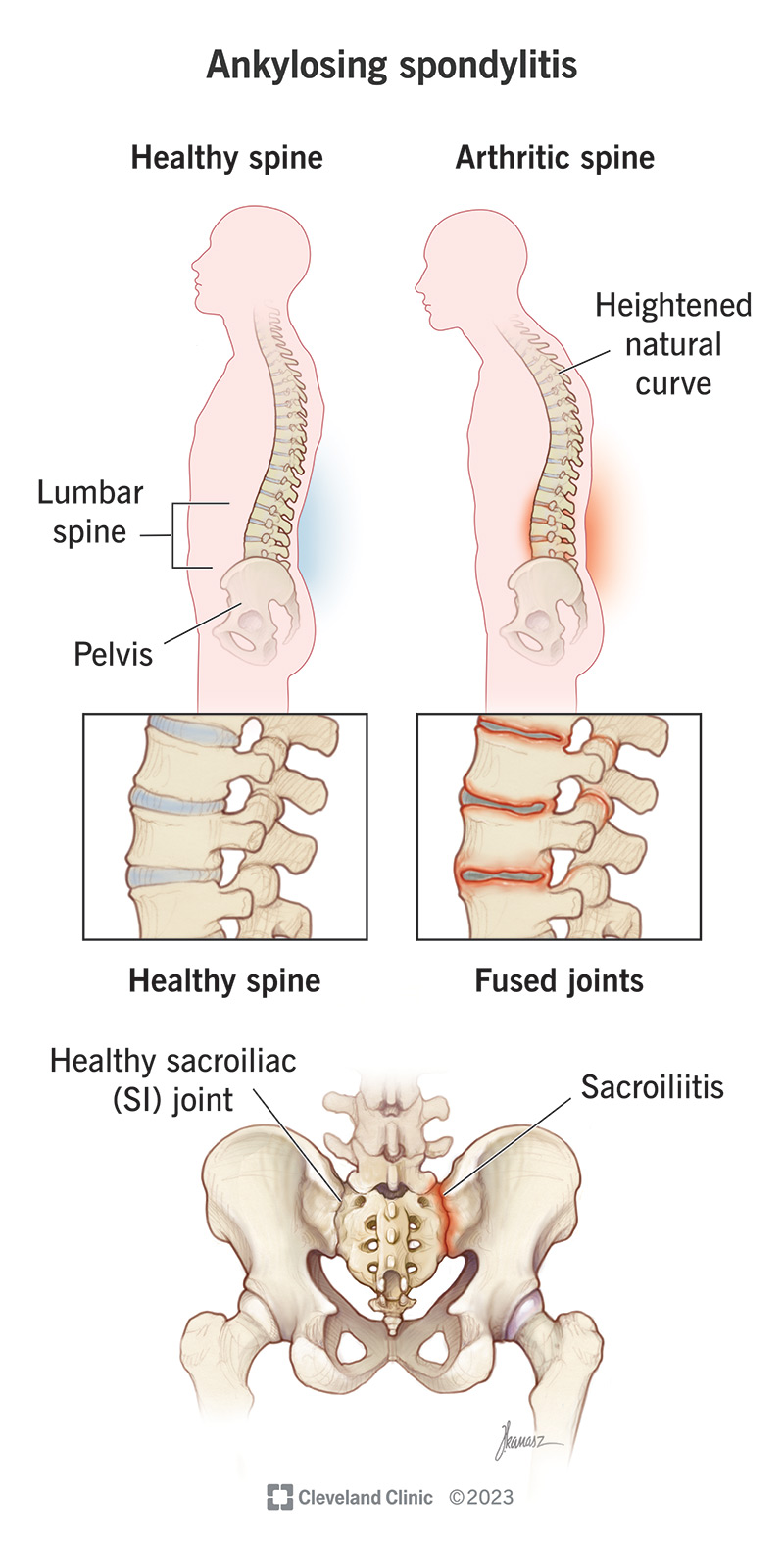
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/ankylosing-spondylitis.jpg)
Ankylosing spondylitis is a type of arthritis that affects joints in your spine. Healthcare providers sometimes call it axial spondylarthritis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Ankylosing spondylitis (AS) also affects the joints where the base of your spine meets your pelvis (your sacroiliac joints). Your sacroiliac joints are the connection between your spine and pelvis. Specifically, they’re the place where the sacrum (the triangle-shaped last section of your spine) meets the ilium (the top and back part of your pelvis).
The sacroiliac joints are some of the biggest joints in your body, and you use them every time you move or shift your hips.
It’s less common, but ankylosing spondylitis can affect other joints, including your:
Ankylosing spondylitis causes pain, stiffness and gastrointestinal (GI) symptoms. Visit a healthcare provider if you’re experiencing lower back pain, especially if it’s getting worse or making it hard to do all your usual daily activities.
Everyone with ankylosing spondylitis experiences a unique combination of symptoms. Lower back pain due to sacroiliitis (painful inflammation in your sacroiliac joints) is the most common AS symptom.
The pain can spread (radiate). You might experience other types of pain, including:
Other ankylosing spondylitis symptoms can include:
Advertisement
Ankylosing spondylitis is an autoimmune disease. Autoimmune diseases happen when your immune system attacks your body instead of protecting it.
Experts aren’t certain what causes ankylosing spondylitis. Studies have found that specific genetic mutations are closely linked to having AS. Genetic mutations are changes to your DNA sequence that happen when your cells divide to make copies of themselves.
There are more than 60 mutated genes that might cause AS. One example is the human leukocyte antigen-B (HLA-B27) gene. More than 90% of white people who have AS also have a mutated HLA-B27 gene.
Anyone can develop ankylosing spondylitis, but certain groups of people are more likely to have it, including:
People with certain health conditions are more likely to have ankylosing spondylitis, including:
People with ankylosing spondylitis have a higher risk of spinal fractures (broken bones in your spine).
Other complications can include:
A healthcare provider will diagnose ankylosing spondylitis with a physical exam. They’ll examine your body and discuss your symptoms. Tell your provider when you first noticed pain or other symptoms, including if any time of day or activity makes them worse.
You might need to visit a rheumatologist, a healthcare provider who specializes in treating arthritis and similar conditions.
There’s no one test that can confirm you have AS. Your provider might use a few tests to help diagnose it, including:
Advertisement
Your healthcare provider will suggest treatments to manage your symptoms and reduce how much they affect your daily routine.
Common treatments for ankylosing spondylitis include:
Advertisement
You should start feeling better soon after starting treatment. Your symptoms might not completely go away, but they should improve as you find treatments that work for you. Ask your provider when to expect improvements. Exercise and physical therapy are a gradual process, and medications take different amounts of time to take effect.
Ankylosing spondylitis is a chronic (long-term) condition. You should expect to manage your symptoms for a long time (maybe the rest of your life). Some people with AS have periods of remission where they have fewer, or milder, symptoms. Even if it’s been a while since you experienced symptoms, there’s always a chance they can come back.
There’s no cure for AS (or any other type of arthritis), but that doesn’t mean you have to live in pain. Talk to your provider about what you’re feeling. Tell them how much your symptoms impact your ability to do your favorite activities.
In addition to following your AS treatment regimen, there are some steps you can take to reduce inflammation in your body and stress on your joints:
Visit your healthcare provider if you notice new symptoms, or if your symptoms get worse. Talk to your provider if it feels like your treatments aren’t managing your symptoms as well as they used to.
Advertisement
See a healthcare provider if you experience any of the following symptoms:
Questions to ask your provider include:
Managing any type of arthritis can be frustrating. If you have ankylosing spondylitis, it’s a literal pain in the back. Pain, stiffness and other symptoms can take a toll on your day-to-day energy levels, but the good news is that AS is manageable.
Your healthcare provider will help you find treatments that reduce how much AS symptoms interfere with your day-to-day routine. Don’t be afraid to ask questions or talk to them about your treatments. You’re the best judge of how you feel.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Low back pain can be a constant interruption in your daily life. Cleveland Clinic’s experts can help craft a treatment plan to help you find relief.
