Juvenile polyposis syndrome (JPS) is a genetic condition that causes recurring growths, called polyps, to form on the lining of your gastrointestinal tract. Screening tests, like an endoscopy or colonoscopy, detect polyps. Removing the polyps reduces symptoms. Early detection and treatment of JPS lead to the best outcome.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
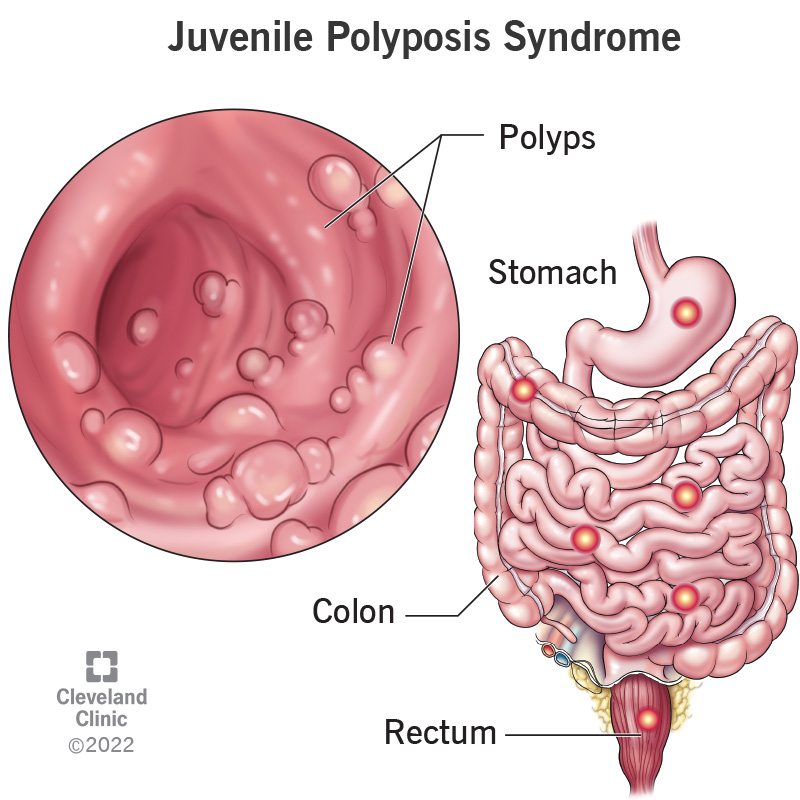
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/juvenile-polyposis-syndrome.jpg)
Juvenile polyposis syndrome (JPS) is a genetic condition where growths, called polyps, form on the lining of your gastrointestinal (GI) tract. These polyps can occur anywhere in your GI tract, most often in your large intestine (colon) and rectum, but they can also grow in the stomach and, more rarely, the small intestine. A person with JPS can have a few polyps or more than a hundred.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are three types of juvenile polyposis syndrome (JPS):
Symptoms typically begin during childhood for generalized juvenile polyposis and juvenile polyposis coli but can affect anyone at any age.
Juvenile polyposis syndrome (JPS) can affect anyone since a genetic mutation causes the condition.
The word “juvenile” refers to the way the polyps look under the microscope, and not to the age of the people who get the condition. However, most people develop symptoms of JPS by the time they are 20 years old.
Yes, you can inherit juvenile polyposis syndrome (JPS). JPS is an autosomal dominant condition, which means only one copy of the gene needs to pass from one parent during conception for you to inherit the condition. An estimated 75% of diagnoses of JPS pass in an autosomal dominant pattern and 25% occur sporadically from new genetic mutations that don’t pass from parents to children.
Advertisement
Juvenile polyposis syndrome affects an estimated one in 100,000 people worldwide.
Juvenile polyposis syndrome might cause symptoms that affect your lower abdomen and bowels. This is most noticeable after you eat or when you go to the bathroom since symptoms can affect your gastrointestinal tract that includes your stomach and rectum. The first sign that you have JPS could be bloody stool (poop). Symptoms could also include abdominal pain or diarrhea. When you first notice symptoms of JPS, visit your healthcare provider. Early detection and treatment of polyps lead to the best outcome. You will need your polyps removed, if possible, to reduce your symptoms and reduce your risk of developing cancer.
The main symptom of juvenile polyposis syndrome is polyps in the gastrointestinal (GI) tract. Polyps are clusters of cells and tissues. These polyps are round and stick out from the wall of your bowel on a stalk and appear as a red to purple color. Polyps form inside of your gastrointestinal (GI) tract, which includes your:
Most of the time, you won’t be able to see your polyps since they form inside your body. On rare occasions, polyps might be visible coming out of your rectum.
Some people diagnosed with juvenile polyposis syndrome don’t experience any symptoms until the polyps increase in size or multiply. Symptoms caused by polyps could include:
Nearly 15% of people diagnosed with juvenile polyposis syndrome experience symptoms other than polyps when they’re born including:
While polyps caused by juvenile polyposis syndrome are benign (non-cancerous), people diagnosed with JPS are at a higher risk of developing certain types of cancer including:
A mutation of the BMPR1A and SMAD4 genes causes juvenile polyposis syndrome (JPS). People with deletions in both _BMPR1A _and another gene called PTEN may present with JPI. The _BMPR1A_ and SMAD4 genes make proteins that create pathways from the cell membrane (the outside wall of the cell) to the nucleus (the center of the cell). These communication pathways are hall monitors that make sure your cells are following instructions to do their job, which is to create new cells that replace old cells.
Advertisement
If you have a mutation of the BMPR1A and SMAD4 genes, there isn’t a hall monitor patrolling the communication pathways to make sure your cells follow the rules. When your cells don’t follow the rules, they copy and divide too frequently, which causes the formation of polyps in your GI tract.
While two different genes cause JPS, you only need one copy of either mutation to get the condition.
People who have a mutation on the SMAD4 gene are at risk of having another condition called hereditary hemorrhagic telangiectasia (HHT).
Your provider will diagnose juvenile polyposis syndrome (JPS) after providing a physical exam and learning more about your symptoms and understanding your family and medical history. They will diagnose JPS if any of the following are true:
If your provider suspects juvenile polyposis syndrome, they will offer a variety of tests to confirm your diagnosis. Tests could include:
Advertisement
Treatment for juvenile polyposis syndrome focuses on removing polyps to relieve symptoms. Your provider will suggest the treatment plan that is right for you based on your age and health, the number of polyps and the location of the polyps. Types of polypectomy procedures include:
Babies and children who have a single juvenile polyp often have it removed during a colonoscopy. Surgery is rare among children to remove polyps unless the polyp is large.
You can manage your juvenile polyposis syndrome (JPS) diagnosis by staying up to date on preventative screenings that monitor your symptoms. Screenings include:
You should schedule tests and preventative screenings when symptoms first appear or before your 15th birthday. If test results are negative, you should repeat screenings every three years.
If your provider only finds a few polyps and removes them or you receive surgery, you should schedule a screening every year unless no polyps are found, then screenings should be done every three years.
Advertisement
After treatment to remove your polyps, your body will need time to heal. You should feel symptoms reduce after a procedure and most people will feel better two weeks after a procedure. This timeframe varies on the number of polyps that your provider removed and how your body recovers.
There is no cure for juvenile polyposis syndrome (JPS). Early detection and treatment of polyps lead to the best outcome and minimize severe symptoms. Polyps will most likely return over time and repeat treatment might be necessary.
People diagnosed with JPS have a 30% to 50% lifetime risk of developing cancer in their GI tract. To reduce your risk, follow your provider’s recommendation to get screenings either annually or every few years.
After a procedure to remove polyps, your provider might suggest a special temporary diet to reduce irritation to your digestive system. It is also important to stay hydrated both before and after a procedure. Talk to your provider to learn more about how you can take care of yourself before and after treatment.
Since juvenile polyposis syndrome (JPS) is a genetic condition, there is no way to prevent it. However, increased awareness, education and screenings help detect polyps, which decreases the risk of symptoms and cancer when treated early.
Call your healthcare provider if you have symptoms of juvenile polyposis syndrome, especially blood in your stool. Be sure to tell your provider if you have a family history of polyps or JPS since it is a hereditary condition.
The International Classification of Diseases (ICD) is a diagnostic tool for healthcare providers to classify conditions for clinical settings. The ICD-10-CM code for juvenile polyposis syndrome is D12.6.
It could be alarming to see blood in your stool. If you do, contact your healthcare provider to get a screening to look for polyps that could cause your symptoms. Detecting and treating polyps early leads to a positive outcome. If you have a history of juvenile polyposis syndrome in your family and you want to better understand your risk of having a child with a genetic condition, talk to your provider about genetic testing.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Kids can get polyps. Sometimes a lot of them. At Cleveland Clinic Children’s, we’ll treat your child’s polyposis syndrome with compassion and expertise.
