Measles is a highly contagious disease that causes a high fever, rash, cough and red eyes. It can lead to life-threatening complications, like brain inflammation and pneumonia. It’s caused by a virus. Getting the measles vaccine is the best way to prevent getting and spreading measles.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy

Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/8584-measles)
Measles is a highly contagious illness caused by a virus. It causes a widespread rash and flu-like symptoms. But measles isn’t just a rash. It can make you severely ill and lead to life-threatening complications like brain inflammation and pneumonia. It can also make you more likely to get sick with other infections.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Before it was part of routine childhood immunizations, measles caused millions of deaths around the world. There are still cases in the U.S. every year. There’s no specific treatment or cure.
Measles is also called rubeola, 10-day measles or red measles. It isn’t the same as German measles (rubella).
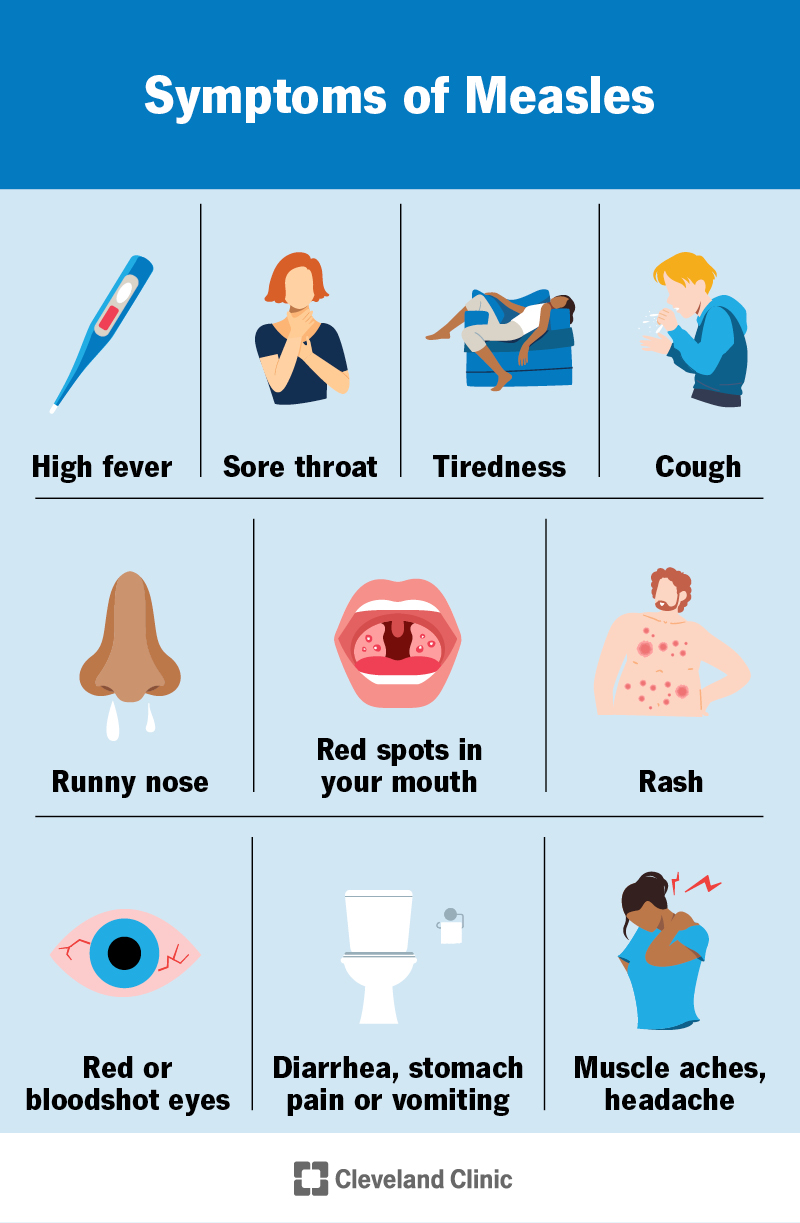
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/8584-measles-symptoms.jpg)
Measles symptoms include:
Measles symptoms don’t appear all at once. A fever, cough, runny nose and red eyes may appear first. Koplik’s spots might appear two to three days later and fade when the rash begins. The rash appears three to five days after your initial symptoms start. A high fever may develop with the rash.
The measles rash usually starts as flat spots on your face. On lighter skin, it appears red. On dark skin, it could appear purple or darker than the skin around it, or it might be hard to see.
The rash spreads downward over your neck, chest, back, arms, legs and feet. The spots might blend together as they spread. There might be some areas that are raised bumps and some that are flat. It doesn’t usually itch.
Advertisement
Measles virus (genus Morbillivirus) causes measles. It’s an airborne disease, which means it spreads through the air when an infected person breathes, coughs, sneezes or talks. The airborne droplets can remain in a room for two hours even after the person with measles is gone. Droplets can also land on surfaces you touch.
Measles can spread by:
Yes, measles is highly contagious, which means it spreads easily from person to person. Experts estimate that if one person in a room of unvaccinated people has measles, 9 out of 10 people in the room will catch it. You’re contagious about four days before you develop a rash until about four days after the rash starts.
You’re at higher risk for severe complications from measles if you:
Complications of measles can be mild to life-threatening. They include:
If you have measles while pregnant, your baby could be born early (preterm birth) or have low birth weight.
A healthcare provider might be able to diagnose measles based on your health history, a physical exam and the appearance of the rash. To confirm a diagnosis, they might use:
There’s no cure and no specific treatment for measles.
If you’re treated in a hospital, a healthcare provider might give you vitamin A to reduce your risk of serious complications. But you shouldn't treat yourself with vitamin A without a healthcare provider watching to avoid organ damage. Too much vitamin A can lead to a serious condition called vitamin A toxicity. Vitamin A won't cure or prevent measles.
Measles usually lasts 10 to 14 days if you don’t have complications.
Advertisement
Talk to your healthcare provider if:
Go to the emergency room if you experience:
Measles can cause severe illness. About 2 out of every 5 people with measles are hospitalized.
Even after you’ve recovered, you might be more likely to get sick with other infections. This is because measles often destroys immune system cells responsible for remembering past infections that you’d developed immunity to (“immune amnesia”).
You can also develop life-threatening complications months or years after having measles, especially if you have a weakened immune system.
Yes, you should isolate for four days after the rash appears if you have measles. You should wear an N95 mask, and so should healthcare providers and anyone who’s helping care for you. Ask your provider when it’s OK to be around other people and return to work or school.
Advertisement
Ask your healthcare provider (or your child’s) how you can safely manage symptoms at home. They might suggest:
The measles vaccine is extremely effective at preventing measles. To be fully protected, you need two doses of either:
Most people get the MMR or MMRV shots in childhood, but you can get them as an adult, too.
It’s unlikely that you’ll get measles if you’ve received both doses of the vaccine. Receiving only one dose is less effective at preventing illness.
Measles once infected nearly every child in the U.S. Thanks to public health efforts, it’s much less common now. But outbreaks still happen, and people still die and have serious complications from measles. If you think you’ve been exposed to measles, talk to a healthcare provider. They can let you know how to manage your symptoms and if there are any ways to reduce your risk of severe illness.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
As your child grows, you need healthcare providers by your side to guide you through each step. Cleveland Clinic Children’s is there with care you can trust.
