A vasectomy reversal is a surgery that allows sperm to pass into your semen and make pregnancy possible. The procedure may take up to four hours to complete. The success rate depends on many factors, including how long it’s been since you had a vasectomy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
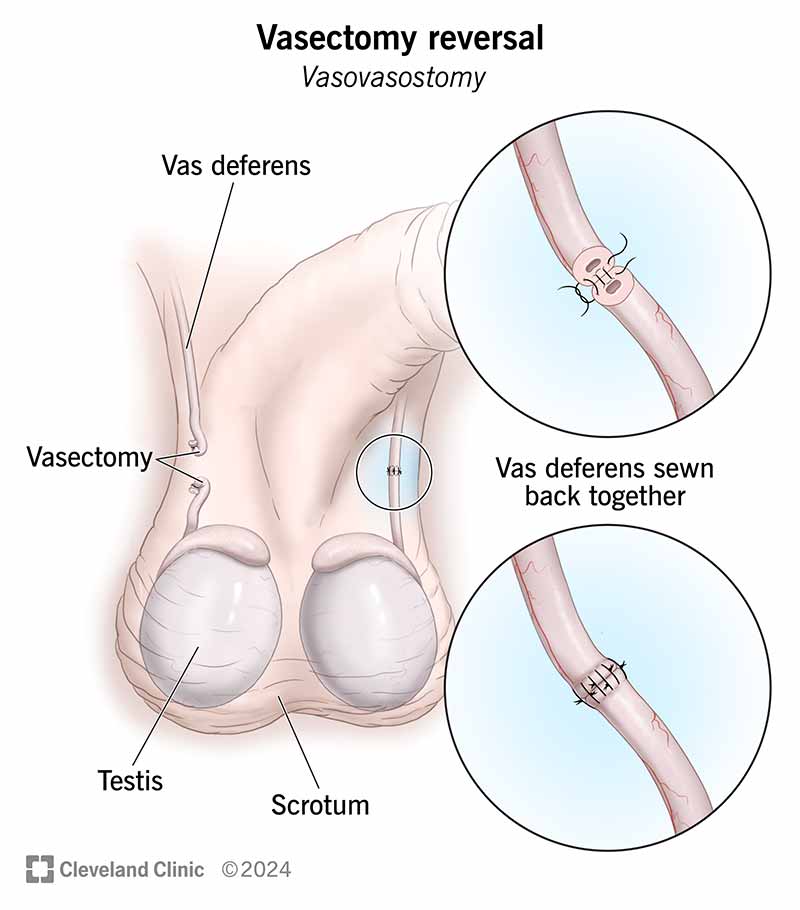
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15459-vasectomy-reversal)
A vasectomy reversal is a surgical procedure that reverses the results of a vasectomy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A vasectomy is a type of surgical birth control. It involves cutting and blocking your vas deferens — the tubes that carry your sperm cells to your semen. During the procedure, a surgeon will remove scar tissue from both ends of your vas deferens. Then, they’ll align the two ends of the tube and sew them together. In some cases, this isn’t possible. So, they’ll sew the vas deferens to your epididymis (ep-uh-DID-uh-miss). Your epididymis is a coiled tube behind each testicle that stores and carries sperm.
Healthcare providers sometimes call a vasectomy reversal a vasovasostomy (vas-oh-va-SOS-tuh-mee).
There are many personal reasons why you may wish to undo a vasectomy. These include:
Advertisement
Before a vasectomy reversal, you should talk to a healthcare provider about the procedure. They may ask you the following questions:
They’ll also evaluate your general health, including any health conditions or risk factors. Tell them about any prescription or over-the-counter medications you’re taking. This includes herbal supplements. Aspirin, anti-inflammatory drugs and certain herbal supplements can increase your risk of bleeding.
Your overall health, comfort and safety are important. It’s a good idea to ask your healthcare provider the following questions during your initial meeting (consultation):
Healthcare providers may ask you to shave the hair from your entire scrotum or groin area the night before or the morning of your procedure.
Don’t use an electric razor on your scrotum. You should only use electric razors to shave your facial hair. They may cause cuts or irritation (razor burn) on your scrotum. A single-blade disposable razor is the best choice.
A special team of healthcare providers perform a vasectomy reversal. The team typically includes:
The anesthesiologist will give you anesthesia, so you won’t feel any pain. They may give you general or local anesthesia. General anesthesia makes you sleep through the procedure. Local anesthesia numbs the area without putting you to sleep.
Once you’re asleep or numb, the urologist will:
Advertisement
A vasectomy reversal may take up to four hours.
Most vasectomy reversals are outpatient procedures. That means you can go home the same day you have your surgery.
After your vasectomy reversal is complete, a healthcare provider will cover your stitches with bandages. The anesthesiologist will also stop putting anesthesia into your body to keep you asleep.
You’ll then move to a recovery room. Nurses will wait for you to wake up, manage your pain and monitor your overall health.
Once they determine you’re OK and no longer need monitoring, they’ll let you go home (discharge you).
The most important benefit of a vasectomy reversal is that it increases your chances of getting your partner pregnant through sexual intercourse.
Other advantages include:
Advertisement
Depending on how many years have passed since your vasectomy, the success rate ranges from 60% to 95% for sperm to return to your ejaculate. Pregnancy is possible for about half of all people after the procedure. But the effectiveness starts to go down around 15 years after a vasectomy.
Even if a vasectomy reversal is successful, other factors contribute to your pregnancy chances. These may include the health of your sperm and your partner’s age. Healthcare providers may recommend fertility tests if you’re having difficulty conceiving.
A vasectomy reversal may not be successful if you have other conditions that affect your testicles. You may also develop blockages after surgery that prevent fertility. Talk to a healthcare provider if you’re still having difficulty conceiving a child after a vasectomy reversal. You may need a second vasectomy reversal or another type of surgery to collect sperm from your testicles.
Other risks may include:
Most people describe the pain after a vasectomy reversal as moderately painful — it’s similar to getting a vasectomy. You can help manage your pain by icing the area and taking OTC pain relievers.
Advertisement
Most people can resume normal activities about two days after a vasectomy reversal. It’s a good idea to wear an athletic supporter (jockstrap) for at least a week after the procedure.
Avoid strenuous activities for at least one week, including running or heavy lifting. You should also avoid sexual activity — including masturbation — for two to three weeks after the procedure.
Over-the-counter (OTC) nonsteroidal anti-inflammatory drugs (NSAIDs) help provide relief for mild pain. The most common NSAIDs include:
Not everyone can take NSAIDs. It’s a good idea to check with a provider before use. If you have a lot of pain, providers may suggest a stronger pain reliever.
You should apply ice packs to the area off-and-on for at least 24 hours after a vasectomy reversal. Don’t ice the area for more than 20 minutes at a time. You also shouldn’t apply ice directly to your skin — wrap it in a towel.
Your body needs time to heal after a vasectomy reversal. It’s a good idea to take between five and seven days off work or school. Ask your provider about when it’s OK to return to work or school.
If you have a physically demanding job, you may need up to two weeks to recover before returning to work.
Vasectomy reversals are generally more successful the sooner they occur after a vasectomy. Success rates often decline over time.
A vasectomy reversal can be a difficult procedure. The input of a urologist with a lot of experience in vasectomy reversals is invaluable. Your success rate also depends on other factors, including:
After a successful vasectomy reversal, sperm should appear in your semen within a few weeks after the procedure.
For most people — more than 80% — vasectomy pain goes away after a successful reversal.
Schedule a follow-up appointment with your urologist. They’ll want to check your incision and take your stitches out after about a week.
You should then schedule a semen analysis six to eight weeks after your vasectomy reversal. A healthcare provider will examine your semen sample under a microscope to evaluate your:
It’s best to collect a semen sample between 48 and 72 hours after your last sexual activity (masturbation or sexual intercourse) to have the greatest sperm cell level.
A vasoepididymostomy is another type of vasectomy reversal.
In some cases, blockages occur in other sperm tubes (pathways) in your body. A urologist may discover these blockages while performing your vasectomy reversal. They must avoid (bypass) the blockage to restore your fertility.
Blockages often occur in your epididymis. As years go by after your vasectomy, you’re more likely to develop this blockage in your epididymis.
After a vasectomy, your testicles still make sperm. But your body absorbs them. Over time, your testicles may produce more sperm than your body can absorb, creating pressure in your vas deferens and epididymis. This pressure may cause a tear (rupture), which a urologist may only discover during surgery.
Urologists perform vasoepididymostomies to bypass the blockage. It’s sometimes a more challenging procedure than a standard vasectomy reversal. But it’ll increase your likelihood of fertility.
If you have a vasoepididymostomy, it’ll take longer for sperm to appear in your semen. It may take up to 15 months.
According to a 2016 study, around 3% to 6% of people who get a vasectomy later choose to reverse it. Even though it’s a rare procedure, the success rate is good.
There’s no time period in which it’s too late for a vasectomy reversal to work. But the success rate tends to drop around 15 years after a vasectomy.
According to a 2020 study, people over 50 who had a vasectomy reversal had the same pregnancy rate as people under 50.
Getting a vasectomy is a big decision. You may have had the procedure because you didn’t think you wanted biological children, or maybe you weren’t yet in a place in your life where it made sense to have a child. But many people who have had a vasectomy change their minds and wish to reverse the procedure.
Getting a vasectomy reversal is also a serious decision. If you’re considering a vasectomy reversal, it’s important to first talk with your spouse or partner about your thoughts. Then, you should schedule an appointment with a healthcare provider. They can explain your options so you can choose what’s best for you and your family.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
There are several reasons for choosing to get a vasectomy reversal. Cleveland Clinic’s expert urology providers will make sure you get the best care possible.
