
As Jennifer Chase entered the third trimester of her pregnancy, her baby boy was growing bigger inside of her. So, too, was an abnormal vein located in the fourth ventricle, a fluid-filled section in the back of her brain. It was the cause of severe dizziness and double-vision. The larger the vein swelled, the more it threatened the life of 37-year-old Jennifer, and her unborn child, Wesley.
Her rare condition — a complex, tangled web of arteries and veins called an arteriovenous malformation (AVM) – occurs in less than 1 percent of the population. And its incidence is even rarer in an otherwise healthy young woman who happens to be pregnant.
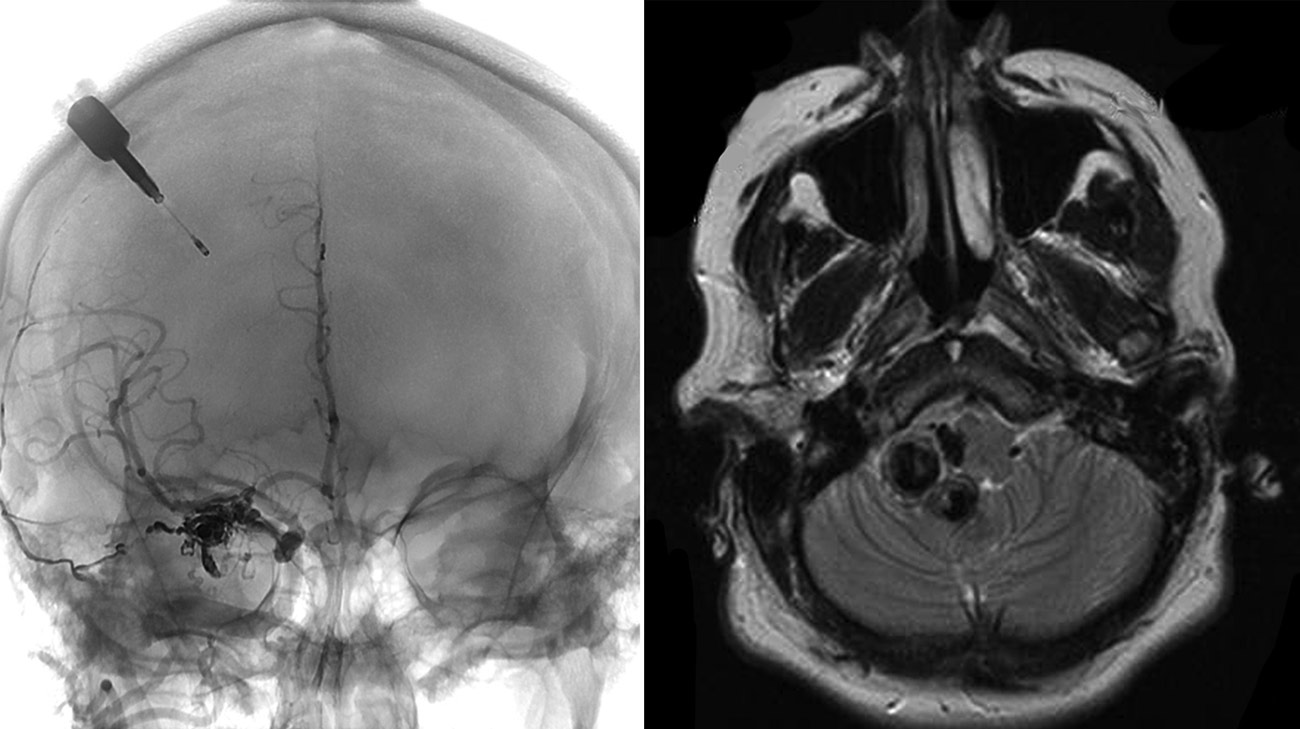
Cleveland Clinic doctors diagnosed Jennifer with arteriovenous malformation (AVM), a tangled web of arteries and veins in her brain. (Courtesy: Cleveland Clinic)
“When I was diagnosed, I had no idea what to expect. I remember thinking, ‘What the heck is an AVM?” she recalled. A multidisciplinary team of Cleveland Clinic physicians explained her condition and treatment options. “That’s when I realized I might have the baby early.”
The specialists involved in Jennifer’s case contended with a vexing quandary: The longer they delayed a premature delivery, the better Wesley’s chances of facing fewer complications. But Jennifer’s troublesome vein could rupture and hemorrhage at any moment, increasing the risk of serious neurological problems or even death.
According to neurosurgeon Mark D. Bain, MD, he and his colleagues (Katherine Singh, MD, a maternal fetal medicine specialist, and Thomas Masaryk, MD, a diagnostic radiologist) contemplated several treatment scenarios before deciding a course of action.

To monitor the pressure in her brain, Cleveland Clinic doctors drilled a hole in Jennifer's skull while performing a C-section. (Courtesy: Shobana Rajan, MD, Cleveland Clinic)
“This case was at the top of the complexity scale. There’s no textbook for it,” Dr. Bain said. “A combination of factors, especially her pregnancy, escalated the complexity and the risk that goes along with it. That’s why we needed to draw on multiple areas for collaboration.”
Ultimately, the team chose a three-phase strategy. First, the neurosurgery team drilled a tiny hole in Jennifer’s skull and inserted an intracranial pressure (ICP) device to monitor her brain’s level of cerebrospinal fluid (CSF) pressure. If a spike in pressure occurred, signaling the AVM may be worsening, the doctors would be aware immediately and be able to take action to reduce the risks.
Next, the team performed a caesarean section at Cleveland Clinic’s Special Delivery Unit, waiting for as long as possible to enable the best outcome for Wesley. Unlike a conventional delivery, Jennifer was put under anesthesia, another attempt to reduce the likelihood of an increase in pressure during the birth.
“By taking these steps, we felt we were doing all we could to ensure the best neonatal outcome,” explained Dr. Singh. “But we knew, if her symptoms got worse, we might have to change our plan immediately.”

Wesley spent 45 days in the NICU. (Courtesy: Jennifer Chase)
Fortunately, Wesley was delivered without incident and was immediately admitted to Cleveland Clinic Children’s Neonatal Intensive Care Unit (NICU), a normal procedure for a premature birth.
A day later, Dr. Bain could at last treat Jennifer’s AVM. He performed a minimally invasive embolization, inserting a small catheter into an artery in Jennifer’s groin and then feeding it up through a series of arteries to her brain, getting as close to the AVM as possible.
The procedure requires the use of X-rays and contrast agents (a dye-like substance that improves visibility of arteries and veins) - another reason the team chose to delay the AVM until after Wesley was born. Using a glue-like obstructive material called Onyx, he sealed off the worrisome vein, enabling her blood flow to reroute through healthier tissue.
The procedure worked perfectly, and a few days later, Jennifer returned home. After 45 days - and countless 360-mile roundtrips by Jennifer and her husband, Chris, to visit Wesley - their son joined them in Parkersburg. Jennifer is back at work, part-time, and the new family is at last experiencing some normalcy.
“We’ve been through so much, but we’ve had wonderful support every step of the way,” said Jennifer, “from the doctors and our family.”
As her first Mother’s Day nears, Jennifer is delighted by what Chris called “the greatest gift of all: having them in good health.”
“Wesley is the sweetest guy,” Jennifer exuded. “He’s so happy and likes to laugh. We’ve been so blessed.”
Related Institutes: Neurological Institute, Ob/Gyn & Women's Health Institute

