Interstitial lung disease (ILD) is a term for a group of conditions that cause inflammation and scarring in your lungs. Symptoms of ILD include shortness of breath and a dry cough. ILD can be caused by medication, radiation therapy, connective tissue diseases or inhaling harmful substances. Lung damage caused by ILD is often irreversible.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
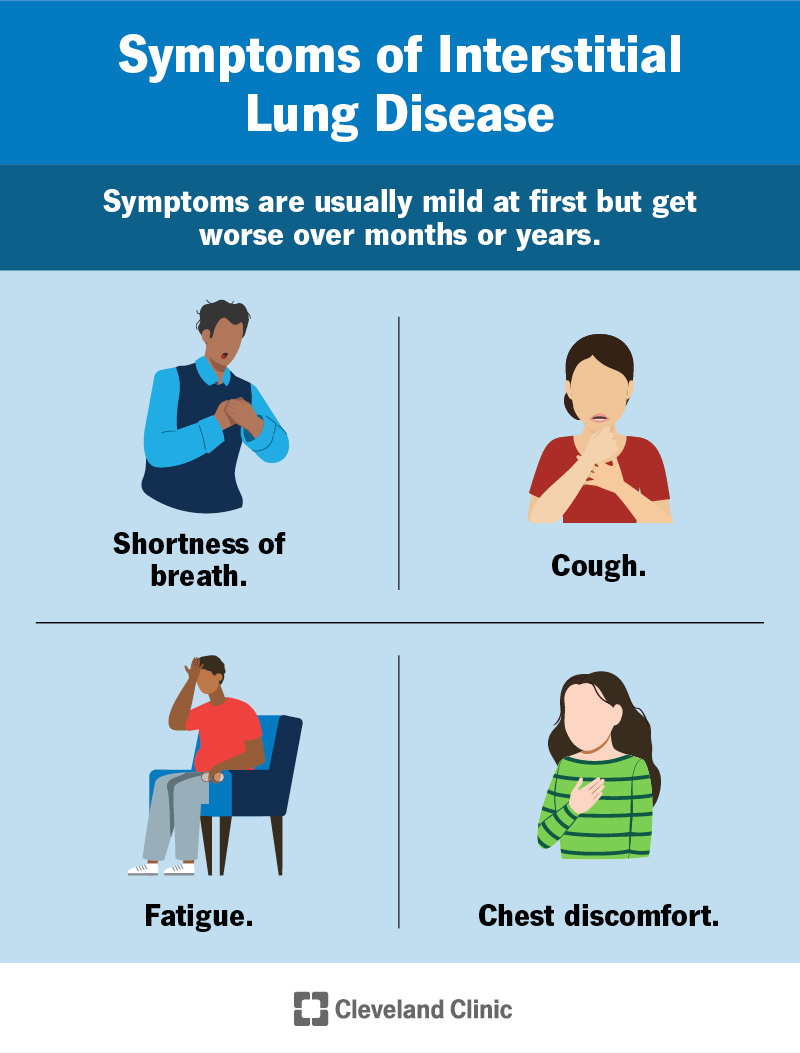
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17809-interstitial-lung-disease)
Interstitial lung disease (ILD) is a term for a group of over 200 conditions that cause inflammation and scarring in your lungs. ILD damages the tissues between the small air sacs in your lungs (alveoli) and the blood vessels around them. This makes it harder for you to move oxygen out of your lungs and into your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Interstitial lung disease is also called diffuse parenchymal lung disease (DPLD).
When you have interstitial lung disease, parts of your lungs that help oxygen get into your blood and out to your tissues are damaged. Scarring in your lungs makes it hard to breathe, and you might have a chronic cough. Lack of oxygen can make you feel tired all the time.
When damage continues to get worse, you can have life-threatening complications, like lung infections and respiratory failure (not enough oxygen or too much carbon dioxide in your body).
There are over 200 interstitial lung diseases. The most common is idiopathic pulmonary fibrosis, followed by diseases caused by occupational exposures or connective tissue disorders. A few other examples include:
Pulmonary fibrosis is a type of interstitial lung disease. Not all ILD is pulmonary fibrosis.
You’re more likely to develop interstitial lung disease if you:
Advertisement
Since there are many kinds of interstitial lung diseases, any one case could be mild or very serious. Most kinds of ILD cause irreversible lung damage. The most serious ILDs are progressive, where your condition continues to worsen over time.
Common symptom of interstitial lung disease include:
Symptoms are usually mild at first but get worse over months or years. You may have additional symptoms depending on the underlying cause of ILD.
The causes of interstitial lung disease are usually described as known or unknown. A known cause is when ILD happens because of a disease you’re living with or something you were exposed to, like certain medications, radiation or harmful substances.
An unknown cause (idiopathic) is when you have ILD but you don’t have an underlying condition and haven’t been exposed to anything to cause it.
Known causes of interstitial lung disease include:
When your healthcare provider can’t find the cause of interstitial lung disease, it’s called idiopathic interstitial pneumonia. There are many types of idiopathic interstitial pneumonias. The most common ILD with an unknown cause is idiopathic pulmonary fibrosis.
Your healthcare provider will diagnose interstitial lung disease by doing a physical exam, getting imaging of your lungs and testing your lung function. During your exam, they’ll listen to your lungs for any unusual sounds that tell them your lungs aren’t working right. They’ll ask you about:
Tests your provider may perform to diagnose interstitial lung disease include:
Advertisement
There’s no cure for interstitial lung disease. Treatment for ILD usually focuses on treating underlying disease and improving your symptoms. Your healthcare provider might prescribe physical therapy, supplemental oxygen or medication to reduce inflammation or slow down the disease.
Some treatments for interstitial lung disease can weaken your immune system. Your provider will monitor you closely for complications if you’re taking one of these medications.
Advertisement
How you and your healthcare provider manage interstitial lung disease depends on the cause. If you have an occupational exposure or allergy (hypersensitivity pneumonitis), you may have to stop working with whatever’s causing your ILD or take extra precautions.
While medications can help bring down inflammation, scarring caused by interstitial lung disease is permanent. If you have an underlying disease, management of it might help prevent further damage. If the cause is unknown, your healthcare provider will treat your symptoms and try to prevent more damage.
In severe cases of interstitial lung disease, you can have life-threatening complications, including:
The life expectancy for interstitial lung disease depends on the cause and severity. Some people with mild ILD can live normal lives without treatment or with minimal treatment. Your outlook (prognosis) is better if your disease isn’t getting worse (it’s stable).
For people with the most severe and rapidly worsening forms of interstitial lung disease, life expectancy is around 3-5 years after diagnosis.
Advertisement
Many causes of interstitial lung disease aren’t preventable. You can reduce your risk of ILD by managing underlying conditions and avoiding breathing in harmful substances.
If you’ve been diagnosed with interstitial lung disease, the best way to take care of yourself is to make a plan with your healthcare provider to manage your symptoms and prevent further damage.
Treat any underlying conditions, and manage anything that could contribute to ILD (like GERD). If you work with substances that can damage your lungs or cause an ongoing allergic reaction, you may need to take special precautions.
See your healthcare provider if you’ve had increasing shortness of breath, shortness of breath with exercise or an ongoing dry cough. The outlook for interstitial lung disease is best if treated as soon as possible.
There are dozens of types of interstitial lung disease. Some cases are mild, and some are very serious. You might find some scary statistics online, but only your healthcare provider can tell you what to expect in your specific case. Having honest conversations with your provider can help set your expectations. Together, you can make a plan to improve your symptoms and have the best quality of life.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When breathing stops being natural and becomes difficult, it’s time to get help. Cleveland Clinic’s interstitial lung disease experts can help manage your symptoms.
