Emphysema is a lung disease. The main cause of emphysema is smoking, but other causes include chemical fumes and toxins in the air. Symptoms include shortness of breath, coughing and fatigue. Your healthcare provider can diagnose emphysema through imaging and breathing tests. Treatment includes quitting smoking and taking medications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
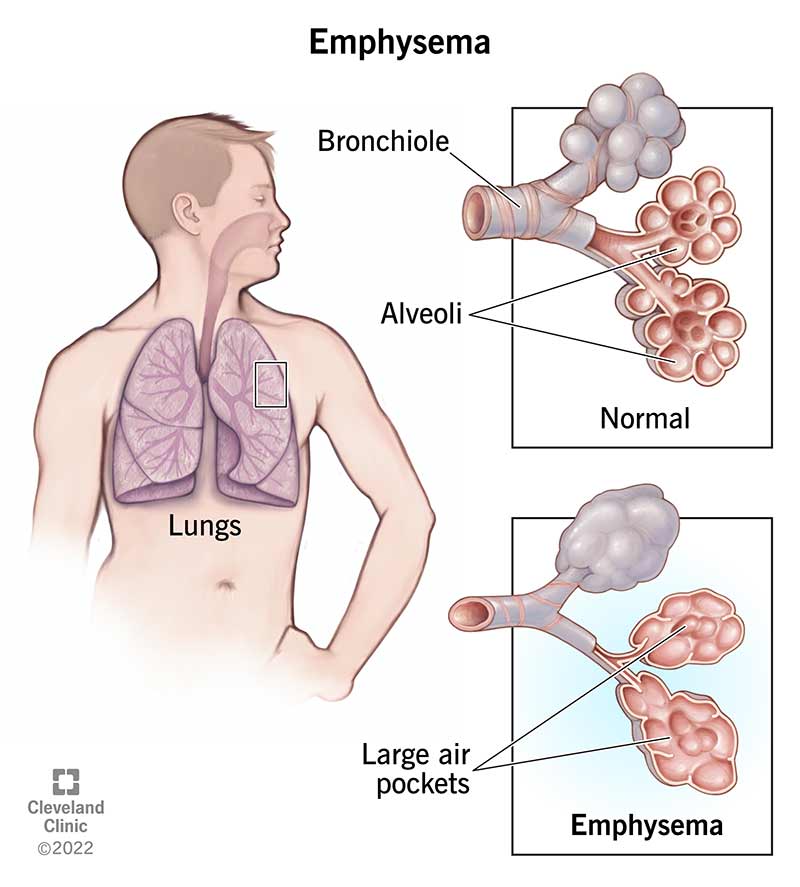
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9370-emphysema)
Emphysema is a lung disease that results from damage to the walls of the alveoli in your lungs. A blockage (obstruction) may develop, which traps air inside your lungs. If you have too much air trapped in your lungs, your chest may appear fuller or have a barrel-chested appearance. With fewer alveoli, less oxygen moves into your bloodstream.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Alveoli are small, thin-walled, fragile air sacs arranged in clusters at the end of the bronchial tubes (airways) deep inside your lungs. In a typical set of lungs, there are about 300 million alveoli. As you breathe in air (inhale), the air travels through the bronchial tubes until it reaches the alveoli. Once the air gets there, the alveoli stretch, draw in oxygen and transport oxygen to your blood. As you breathe out air (exhale), your alveoli shrink and force carbon dioxide out of your body.
Think of your lungs as bubble wrap. The alveoli are like individual bubbles in bubble wrap. If you have emphysema, your alveoli eventually break. Instead of many tiny bubble wrap bubbles, you develop a large air pocket, like a big shipping air pillow. This damage causes your lungs’ overall surface area to shrink, and it makes it hard to get fresh air in and out of your lungs. This makes your breathing difficult and makes you short of breath.
Emphysema usually develops after many years of smoking. However, emphysema has other causes. These include:
Over 3 million people in the United States have emphysema.
Advertisement
Chronic obstructive pulmonary disease (COPD) is an umbrella term that includes a range of progressive lung diseases. These diseases include emphysema and chronic bronchitis. Sometimes people with COPD also have asthma.
Emphysema and chronic bronchitis are both types of COPD. Many people have them both at the same time.
Emphysema is a lung disease that damages the alveoli in your lungs. The primary symptom of emphysema is shortness of breath.
Chronic bronchitis is a lung condition that destroys the cilia in your airways. Cilia are hair-like parts (organelles) of cells that move germs and other debris out of your airways. The primary symptom of chronic bronchitis is mucus production, including a wet cough that produces thick, discolored (yellow, green or yellow-grey) mucus from your lungs (productive cough). Emphysema has more symptoms, including shortness of breath and cough.
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) categorizes COPD in four stages. Emphysema is a cause of COPD, but not all patients with emphysema have COPD. Healthcare providers use the COPD stages to help describe emphysema. The stages are:
Life expectancy varies according to your age and stage of emphysema. Whether you smoked, used to smoke or never smoked also factors into your life expectancy. Smoking reduces your life expectancy by 3.5 years. Genetic factors also play a role in your life expectancy.
Males between 50 and 70 are the most likely group to have emphysema. Medical studies on how emphysema and smoking reduce the life expectancy of 65-year-old males show:
| Stage | Reduction in life expectancy for people who smoke | Reduction in life expectancy for people who used to smoke | Reduction in life expectancy for people who never smoked |
|---|---|---|---|
| 1 | 3.8 years | — | — |
| 2 | 5.7 years | 4.9 years | 0.7 years |
| 3 | 9.3 years | 4.9 years | 1.3 years |
| 4 | 9.3 years | 9.1 years | 1.3 years |
| Stage | |||
| 1 | |||
| Reduction in life expectancy for people who smoke | |||
| 3.8 years | |||
| Reduction in life expectancy for people who used to smoke | |||
| — | |||
| Reduction in life expectancy for people who never smoked | |||
| — | |||
| 2 | |||
| Reduction in life expectancy for people who smoke | |||
| 5.7 years | |||
| Reduction in life expectancy for people who used to smoke | |||
| 4.9 years | |||
| Reduction in life expectancy for people who never smoked | |||
| 0.7 years | |||
| 3 | |||
| Reduction in life expectancy for people who smoke | |||
| 9.3 years | |||
| Reduction in life expectancy for people who used to smoke | |||
| 4.9 years | |||
| Reduction in life expectancy for people who never smoked | |||
| 1.3 years | |||
| 4 | |||
| Reduction in life expectancy for people who smoke | |||
| 9.3 years | |||
| Reduction in life expectancy for people who used to smoke | |||
| 9.1 years | |||
| Reduction in life expectancy for people who never smoked | |||
| 1.3 years |
Many people don’t notice emphysema symptoms until the disease has destroyed 50% or more of their lung tissue. Until then, the first signs include gradual shortness of breath and tiredness (fatigue).
Other emphysema symptoms include:
If you have emphysema, you also have an increased risk of pneumonia, bronchitis and other lung infections.
Smoking is the main cause of emphysema.
Cigarette smoke destroys your lung tissue, and it also irritates your airways. Cigarette smoke causes inflammation and damages your cilia. Irritation and damaged cilia cause swollen airways, mucus production and difficulty clearing your airways. All of these changes can cause shortness of breath.
Advertisement
Though smoking is the main cause of emphysema, there are other causes. These include:
No, emphysema isn’t contagious. If you have emphysema, you can’t give it to another person.
Your healthcare provider can diagnose emphysema. However, they can’t diagnose emphysema solely from your symptoms.
Your healthcare provider will perform a physical examination. During the physical exam, they’ll listen to your lung sounds with a stethoscope (auscultation). A stethoscope is a medical device that features a small, metal disc (diaphragm) that connects to earpieces with rubber tubing.
With their stethoscope pressed against your chest, your healthcare provider will tap on your chest and listen for a hollow sound. If they hear a hollow sound, that means your lungs are trapping air. They’ll then order tests to confirm emphysema.
Your healthcare provider may order the following tests to diagnose emphysema:
Advertisement
No, your lungs can’t heal from emphysema. However, treatments can help reduce your symptoms and improve your quality of life. Other interventions can help prevent further damage from occurring.
Emphysema can worsen over time, so treatment focuses on slowing emphysema down and maximizing the function of your remaining healthy lung. The type of treatment depends on the severity of your emphysema.
Treatment options may include:
Advertisement
Your expectations depend on the severity of your emphysema.
If you have mild emphysema, your outlook is better. However, even mild emphysema can still affect some of your abilities, especially if you’re 65 or older. Activities such as walking, climbing stairs or getting dressed may cause symptoms to appear.
If you have severe emphysema, breathing is extremely difficult and you may require regular medical help.
There isn’t a cure for emphysema. Even if you quit smoking, your lungs won’t be able to heal the existing damage. However, you can slow emphysema down with treatment. Your quality of life will be better the earlier you start emphysema treatment.
The best way to reduce your risk of developing emphysema is to avoid smoking.
Quitting smoking is difficult to do. It may take several attempts to quit successfully. When you’re ready to quit smoking, talk to your healthcare provider. They can help you develop a plan to quit smoking. It’s also a good idea to join support groups. Support groups allow you to share your feelings and experiences with those who understand what you’re experiencing.
Other ways to help reduce your risk of developing emphysema include:
If you have emphysema, the best way to prevent or reduce further problems is to quit smoking and avoid respiratory infections. The following tips can help prevent a respiratory infection:
If you have severe shortness of breath, call 911 immediately.
Talk to your healthcare provider if you experience the following:
If you don’t already have diseased or damaged lungs, COVID-19 can cause giant emphysema. However, it’s rare for this to happen, and there are very few cases that link COVID-19 and giant emphysema.
Giant emphysema is a bullous disease. If you have emphysema, the air pockets may grow and affect up to one-third of one or both of your lungs. Providers call these giant air pockets bullae (singular bulla).
Other names for giant emphysema include giant bullous emphysema and vanishing lung syndrome.
Emphysema is a chronic obstructive pulmonary disease that damages the air sacs in your lungs and makes it hard to breathe. You can’t reverse emphysema damage, and it’ll gradually get worse. However, you can manage the symptoms with treatment and slow down the effects of emphysema. In addition to treatment, you’ll breathe easier if you follow tips that prevent respiratory infections. An early diagnosis will help you maintain your quality of life for a longer period. If you have breathing problems, talk to your healthcare provider, especially if you smoke. They can diagnose emphysema and work with you to develop a healthcare plan so you can continue doing the activities you enjoy for as long as possible.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Emphysema can leave you gasping for breath. The experts at Cleveland Clinic can treat emphysema and help you manage it so you can breathe easier.
