Ventricular dyssynchrony is a disorganized contraction of your heart’s lower chambers (ventricles). This doesn’t allow your heart to pump as well as it should. Medicine or pacemakers can help. A pacemaker may provide long-term benefits, including less time in the hospital and longer life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Ventricular dyssynchrony is an uncoordinated beat (contraction) of one or more of your heart’s lower chambers (ventricles). You may have dyssynchrony if you have as little as a 40-millisecond delay in the contraction of various parts of your ventricle or from one ventricle to the other.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your heart works best when your ventricle muscles contract at the same time. Normally, signals go through your heart in an organized way. When your heart’s two ventricles get a signal to contract, the muscles in your ventricles should contract the same amount at the same time. Your left ventricle, which is the main pumping chamber of your heart, needs to contract in a coordinated way, with both sides of the chamber squeezing toward the middle.
When the signal can’t reach both of your heart’s ventricles at the same time, your muscles can’t contract at the same time. This is dyssynchrony.
Ventricular dyssynchrony affects your body in these ways:
The types of ventricular dyssynchrony include:
Advertisement
Ventricular dyssynchrony affects people who have:
As many as one-third of people with a certain type of heart failure get ventricular dyssynchrony. About 2% of adults in developed nations have heart failure. About 6% to 10% of people older than 65 have heart failure.
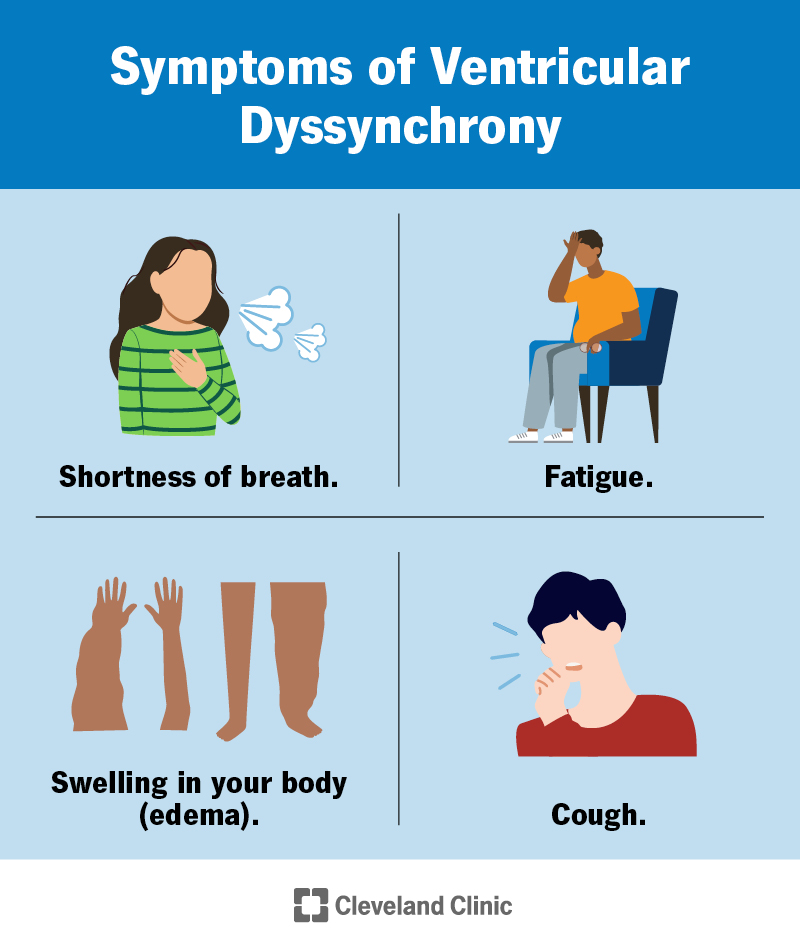
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24279-ventricular-dyssynchrony-cv)
Ventricular dyssynchrony makes symptoms of heart failure more severe or can have symptoms of its own. These symptoms include:
Several different heart issues cause ventricular dyssynchrony, including:
Your provider will evaluate your heart’s function by taking a history and performing a physical exam. Listening to your heart with a stethoscope can uncover ventricular dyssynchrony. An electrocardiogram (ECG) is the most common test for detecting problems with your heart’s conduction system, which are responsible for dyssynchrony in the ventricle. These include right bundle branch block and left bundle branch block. These findings will prompt further evaluation and testing.
Providers often use an echocardiogram to diagnose ventricular dyssynchrony.
Other tests include:
Healthcare providers may treat the condition that’s causing your ventricular dyssynchrony.
In many cases, cardiac resynchronization therapy (which your provider may call CRT or a biventricular pacemaker) can help your heart pump better by pacing the heart from both sides. But it only improves symptoms for 50% to 70% of people who get it. Successful treatment is more likely to happen in those with severe dyssynchrony.
Complications from putting in a CRT (biventricular pacemaker) may include:
CRT decreases ventricular dyssynchrony right away. Some people feel an improvement just a few weeks after having the device implanted. And there are long-term benefits as well, such as:
Advertisement
For dyssynchrony-causing conditions like heart failure, cardiomyopathy or high blood pressure, a provider may prescribe medicines, including:
While these medications will improve the function of your heart, they won’t in themselves reverse dyssynchrony that abnormal electrical conduction causes.
You’re likely to have a poor outcome if you don’t treat left ventricular dyssynchrony. People who have left ventricular dyssynchrony have a higher risk of cardiac events than those who don’t. You can have dyssynchrony in either ventricle (or both), but your left ventricle is the pump that sends oxygen-rich blood to your body. This is a very important job.
The treatment, CRT (a biventricular pacemaker), can help people with heart failure have fewer hospital stays and live longer.
The underlying cause of the dyssynchrony also affects the outlook/prognosis. Some will have a worse outlook than others.
The best thing you can do to reduce your risk is to take good care of your heart. If you do that, you may be able to prevent some of the conditions that cause ventricular dyssynchrony.
Ways to care for your heart include:
Advertisement
If your provider prescribed medicine for you, be sure to keep taking it according to the instructions. Don’t stop taking prescription medication unless your provider tells you to stop.
If you have a biventricular pacemaker, be sure to go to your follow-up appointments. These allow your provider to check that your pacemaker is working correctly. Some hospital systems offer special clinics called CRT clinics, where heart rhythm physicians and heart failure specialists work together to make sure you’re getting the most out of your biventricular pacemaker.
Contact your provider if the medicines they prescribed for you aren’t working. Also, contact them if you’re having trouble with your biventricular pacemaker.
Get medical help right away if you feel:
It’s unsettling to know that your heart isn’t working the way it should. Your provider can find the cause of your dyssynchrony and select the right treatment for you. Be sure to follow the instructions on your medicine bottles. Taking medicine at the same time every day can make it easier to remember. Marking your appointments on a calendar or putting reminders on your phone can help you avoid missing checkups.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
