Inverse psoriasis is an immune-mediated condition. It causes a rash in areas of your skin that rub together, including your groin and armpits. There isn’t a cure, but treatments can alleviate related symptoms, including itching and discoloration.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
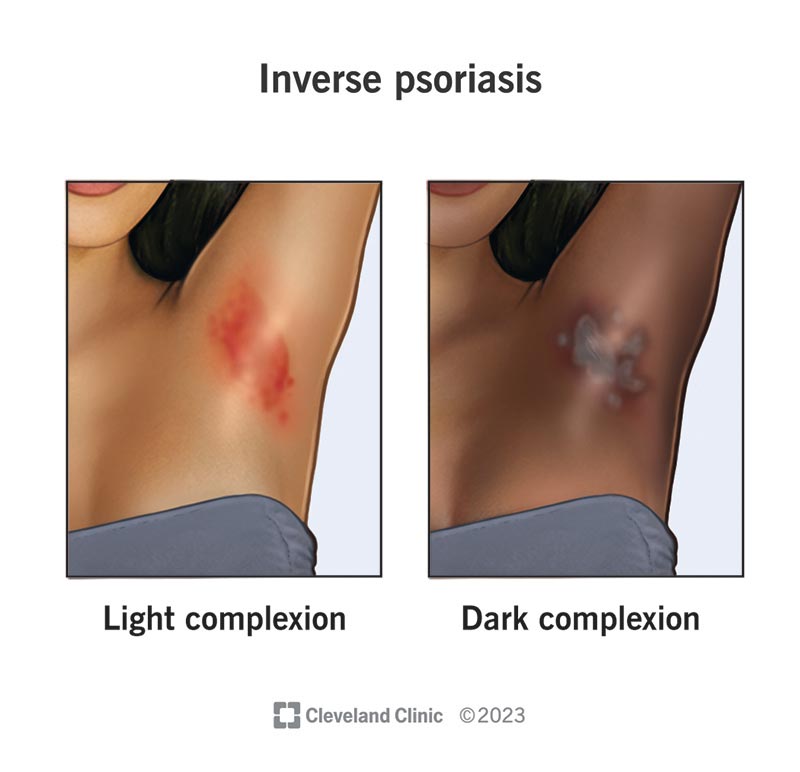
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22852-inverse-psoriasis)
Inverse psoriasis is a disease that causes your skin cells to reproduce very quickly. It’s a type of psoriasis that appears in areas where your skin rubs against itself (skin folds), including:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It looks like a shiny, smooth, discolored (brown, red or purple) rash, and it may feel damp.
Inverse psoriasis is commonly referred to as an autoimmune disease. But the antibody that causes the condition hasn’t been identified. So, it’s technically categorized as an immune-mediated disease. This means the exact cause is unknown, but experts believe it has something to do with your immune system response.
Healthcare providers sometimes call it intertriginous (inter-trij-uh-nus) psoriasis.
Psoriasis and inverse psoriasis are both diseases that affect your skin.
Psoriasis features thick, discolored patches of skin covered with white or silvery scales. The thick, scaly patches are plaques.
Inverse psoriasis doesn’t feature the thick, scaly plaques like other types of psoriasis, most likely because it’s present in moist areas of your body. An inverse psoriasis rash also looks shinier than a psoriasis rash.
Inverse psoriasis and intertrigo are both inflammatory skin conditions that result in rashes in your skin folds. However, inverse psoriasis and intertrigo have different causes and treatments.
Skin rubbing against itself causes intertrigo. Trapped moisture causes the surfaces of your skin to stick together in your skin folds. The moisture increases the friction, which leads to skin damage and inflammation. Keeping the affected area dry, clean and cool can help alleviate intertrigo.
Advertisement
Inverse psoriasis is an immune-mediated disease. That means your body’s immune system attacks parts of your skin instead of protecting your body from foreign invaders like bacteria or viruses. Treatments can help reduce inverse psoriasis symptoms or make them go away. However, inverse psoriasis is a long-lasting (chronic) condition, which means flare-ups can occur throughout your life.
Anyone can get inverse psoriasis. However, you may be more likely to develop inverse psoriasis if you:
Inverse psoriasis can be annoying and painful, but it’s rarely serious. It tends to affect parts of your body where your skin is sensitive.
Scratching your inverse psoriasis rash can break your skin and lead to an infection, which can be more serious to treat.
Psoriasis affects up to 2% of the world’s population and up to 3% of the U.S. population. Between 3% and 7% of those with psoriasis also have inverse psoriasis.
Inverse psoriasis commonly affects sensitive skin areas that rub against each other, such as skin folds. The most common places that inverse psoriasis occurs include:
Moist, sensitive skin areas are more likely to develop inverse psoriasis, so you may be more likely to experience:
Symptoms of inverse psoriasis include:
Symptoms of inverse psoriasis with an infection may include:
Inverse psoriasis is an immune system problem. Your immune response overreacts, causing inflammation, which leads to new skin cells growing too fast.
Typically, new skin cells grow every 28 to 30 days. But in people with inverse psoriasis, new cells grow and move to the surface of your skin every three to four days. The buildup of new cells replacing old cells creates a shiny rash.
Inverse psoriasis runs in families, so there may be a genetic trigger. Parents may pass it down to their children.
Advertisement
Inverse psoriasis flare-ups differ from person to person. No one knows exactly what causes them. Common inverse psoriasis triggers may include:
Inverse psoriasis isn’t contagious. You can’t spread inverse psoriasis to another person through skin-to-skin contact or unprotected sex.
Your healthcare provider will examine your affected areas, and they’ll look for common signs of inverse psoriasis. They’ll also ask about your symptoms, your family history and if you’ve recently started or stopped using a product or medication just before your flare-up.
Your healthcare provider may perform several tests to rule out other conditions that could cause your rash. This is a differential diagnosis. The tests may include:
There isn’t a cure for inverse psoriasis. You may have flare-ups and times where the rash goes away (remission). Treatment can provide relief for your symptoms.
Your healthcare provider may prescribe or recommend the following to help relieve your symptoms:
Advertisement
Several home remedies can help you manage the symptoms of inverse psoriasis.
While home remedies are safe for most people, it’s a good idea to check with your healthcare provider before trying some of the following options. You may be at risk of developing an allergic reaction.
Advertisement
Inverse psoriasis may flare up and go into remission throughout your life. However, it can generally be well managed with treatment.
If you have inverse psoriasis, you may be at a higher risk of:
Inverse psoriasis isn’t a sexually transmitted infection (STI). Still, it can look like an STI. It’s a good idea to be honest with your partner if you have a flare-up. If they have any questions, encourage them to talk to a healthcare provider before you have sex.
If you have inverse psoriasis on your genitals, you may experience discomfort or pain during sex. Sexual lubricants (lubes) and condoms can help ease discomfort, pain or itching.
After sex, carefully clean and dry your genitals and reapply any inverse psoriasis medications.
There isn’t any way to prevent inverse psoriasis. If you have inverse psoriasis, it may come and go throughout your life. Treatments can reduce symptoms, even in people with severe psoriasis.
If you have inverse psoriasis, the best way to take care of yourself is to:
Other steps to stay as healthy as possible include:
Contact your healthcare provider if:
Inverse psoriasis is an immune-mediated disease that causes a rash in areas of your body where your skin rubs against itself. It can make you feel self-conscious, and it can be unpleasant if it itches. However, it isn’t contagious, and treatments can help your symptoms improve.
It’s important to pay attention to your skin. Contact your healthcare provider as soon as you notice a rash.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Coping with psoriasis can be frustrating and distressing. Cleveland Clinic experts offer personalized treatment to help you manage this chronic condition.
