Intertrigo is a common and treatable skin condition that can lead to an infection. It often happens in skin folds where your skin rubs together. The friction causes inflammation that looks like a red, bumpy rash.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
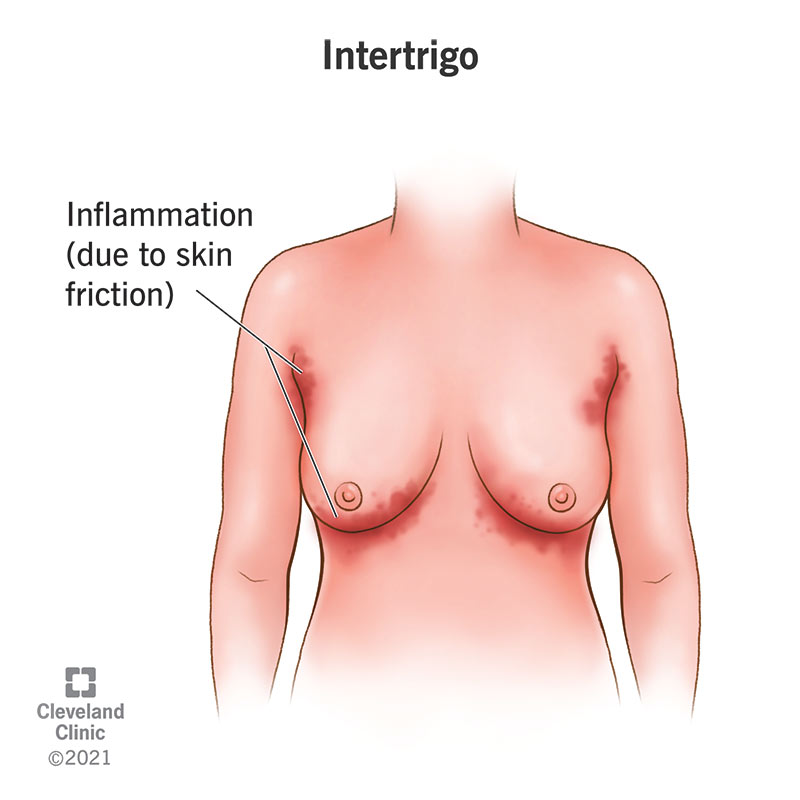
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21693-intertrigo)
Intertrigo is a common inflammatory skin condition that is caused by skin-to-skin friction (rubbing) that is intensified by heat and moisture. It usually looks like a reddish rash. Trapped moisture, which is usually due to sweating, causes the surfaces of your skin to stick together in your skin folds. The moisture increases the friction, which leads to skin damage and inflammation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In many cases of intertrigo, damage to the skin allows bacteria and/or fungus normally present on the surface of your skin to overgrow. The warmth, trapped moisture and friction-induced skin damage create an ideal environment for bacteria and fungi to grow and multiply. This overgrowth of bacteria and/or fungi triggers your immune system to respond, which results in secondary inflammation and a visible rash. In more severe cases, the bacterial and/or fungal overgrowth is significant enough to cause a secondary infection.
Intertrigo itself is not an infection. It’s an inflammatory skin condition. However, intertrigo often leads to a fungal or bacterial infection. This is known as a secondary infection. Candida — a type of yeast, or fungus — is the most common cause of secondary infection related to intertrigo.
Intertrigo can appear in between any skin areas that are in close contact with each other, such as skin folds, and that are often moist.
The most common places that intertrigo occurs include:
Advertisement
Babies are especially at risk for intertrigo because their skin is delicate and they’re more likely to have moist skin from drooling or from wearing diapers. The most common places for babies to have intertrigo include:
There are a few names for intertrigo (also known as intertriginous dermatitis) depending on certain factors such as where it appears and if it’s caused an infection or not. Your healthcare provider may use one or more of these terms to describe your intertrigo:
You can have intertrigo in more than one place on your body at the same time, but intertrigo does not spread to other parts of your body. This is because a key contributing factor for intertrigo is friction from skin-to-skin rubbing, so only places on your body where your skin rubs together can have intertrigo.
If you get an infection from your intertrigo, the infection can spread to other parts of your body and can cause serious complications. It’s important to see your healthcare provider as soon as possible if you have signs of an infection.
Anyone at any age can get intertrigo. Babies often get diaper rash (diaper dermatitis), which is a form of intertrigo. People who have obesity, diabetes and/or a weakened immune system due to underlying disease or medication are more likely to get intertrigo.
Intertrigo is a common skin condition. It’s most common in hot and humid environments and during the summer.
Intertrigo is caused by skin-to-skin friction that is made worse by heat and moisture. This most commonly happens between skin folds or creases and between your toes or fingers.
The trapped moisture — often due to sweating — causes your skin surfaces to stick together. This increases the friction between your skin surfaces, which causes skin damage, bacterial and/or fungal overgrowth and inflammation. In many cases of intertrigo, the skin breaks open from the friction, which allows bacteria and/or fungus to get into your skin, causing an infection. The moisture and warmth make a perfect environment for bacteria and fungi to multiply. If the affected area comes in contact with sweat, pee or poop, it can make your intertrigo worse.
Advertisement
Different kinds of fungi and bacteria that can cause secondary infections include:
Signs and symptoms of intertrigo depend on how severe it is and if there is an infection or not.
Early symptoms of intertrigo without infection can include:
If intertrigo is not treated in its early phase, you can develop the following symptoms:
Advertisement
Symptoms of intertrigo with an infection can include:
If you have signs of an infection, it’s important to see your healthcare provider or go to the nearest hospital as soon as possible. Infections need proper medical treatment and can lead to serious complications if they’re left untreated.
Intertrigo is not contagious. You can’t get it from another person or spread it to another person.
Even though intertrigo is a common condition, it can be difficult to diagnose because it can look like other skin conditions that can affect skin folds. Your healthcare provider will ask you thorough questions about your history, focusing on any skin conditions you currently have or have had in the past. They’ll also ask you questions about medications you take, allergies and sensitivities you may have and if you’ve used certain kinds of topical ointments or soaps. They’ll then do a visual examination of your affected skin.
If your provider suspects you have an infection from your intertrigo, they may perform certain tests such as a skin scraping to see what kind of organism is causing the infection.
Advertisement
There’s currently no formal test or assessment tool to diagnose intertrigo. Your healthcare provider will diagnose your intertrigo based on thorough questions about your history and a visual exam of your affected skin.
If your healthcare provider thinks you may have an infection from your intertrigo, they may perform one or more of the following tests:
The main way to treat intertrigo that hasn’t caused an infection is by keeping the affected area dry, clean and cool.
Ways you can keep your intertrigo dry, clean and cool at home include:
Other things you can do to treat uninfected intertrigo include:
Treatment for intertrigo that has caused an infection depends on what caused it. Your healthcare provider will need to find out what kind of bacteria or fungi have caused your infection in order to give you proper treatment.
Treatment for infected intertrigo can include:
While intertrigo can be unpleasant and painful, it is treatable. The prognosis (outlook) for intertrigo depends on the person’s overall health. In most cases, people recover well from intertrigo if it’s treated properly.
Intertrigo can become chronic (long-lasting) or recurrent (occurring often), so it’s important to take care of yourself and follow a proper hygiene routine to prevent your intertrigo from coming back.
If intertrigo is not treated properly, it can cause complications, including:
Risk factors for getting intertrigo include:
There are several things you can do to try to prevent getting intertrigo, including:
If you’ve had repeated cases of intertrigo, the following actions may help to prevent future cases:
If you have a skin rash that isn’t going away or suddenly gets worse, it’s important to see your healthcare provider. There are many different kinds of skin rashes — many of which look very similar —so your provider will want to make sure your rash is in fact intertrigo and not something else.
If you have been diagnosed with intertrigo and your intertrigo doesn’t seem to be getting better with treatment, contact your healthcare provider.
If you have signs of an infection from your intertrigo — such as a foul smell in the affected area or pus—be sure to see your healthcare provider as soon as possible or go to the nearest hospital. Infections need proper medical treatment.
If you’ve had multiple cases of intertrigo over time (recurrent intertrigo), talk to your healthcare provider about how you can prevent it from coming back and more permanent solutions for prevention.
While intertrigo can be unpleasant and painful, the good news is that it’s treatable and often preventable. Try your best to prevent intertrigo by keeping your skin clean, dry and cool, especially if you’re at a higher risk of getting it. If you have symptoms of intertrigo, be sure to contact your healthcare provider. You will receive a proper diagnosis and a treatment plan so that you can feel better soon.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
