Landau-Kleffner syndrome (LKS) is a rare brain condition that causes children to lose their ability to speak and understand language. Children with LKS have unusual electrical activity in their brain, and many also experience seizures. Healthcare providers may treat LKS with medication, speech therapy and behavioral therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Landau-Kleffner syndrome (LKS) is a rare brain condition that makes children lose their ability to speak and understand language. Healthcare providers sometimes call this condition acquired aphasia with epilepsy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
LKS causes abnormal electrical activity in your child’s brain. Symptoms usually start between 3 and 8 years old. But it can develop at any age, including into the teen years.
In 2022, experts updated the way they group and name certain epilepsy-related conditions. Landau-Kleffner syndrome is now considered a specific type of a broader category called epileptic encephalopathy with spike-wave activation in sleep (EE-SWAS). This means LKS is part of a group of conditions that involve unusual brain wave activity during sleep and problems with speech, language or learning.
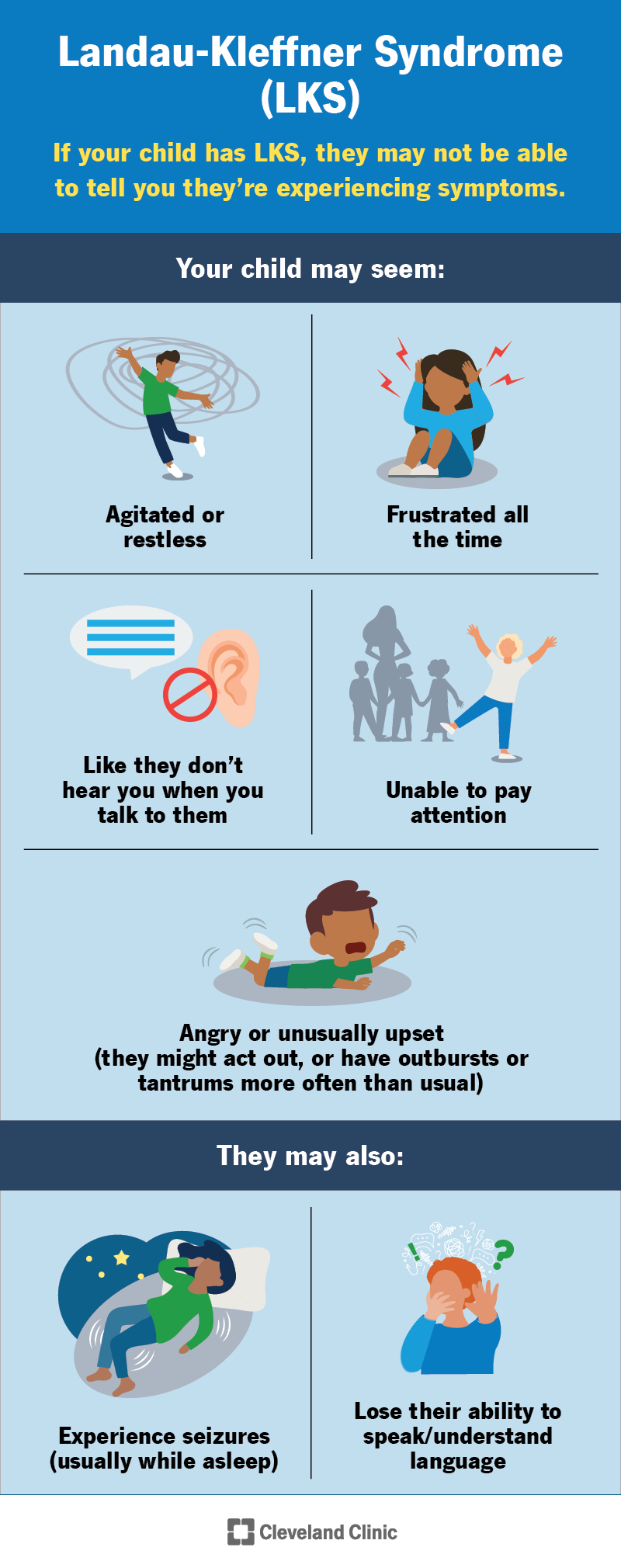
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/landau-kleffner-syndrome)
Children with Landau-Kleffner syndrome may lose their ability to speak (aphasia) and understand language (auditory agnosia). This can happen suddenly or slowly over time. Most children with LKS also have seizures, usually while they’re sleeping.
If your child has this syndrome, they may not be able to tell you they’re experiencing symptoms (especially if they’re having a hard time communicating). You may notice changes in their mood or behavior. Your child may seem:
Advertisement
The unusual electrical activity in their brain may lead to other conditions, including:
Experts are still trying to figure out what causes Landau-Kleffner syndrome. Researchers think it may be a genetic condition or an autoimmune disease.
Researchers found that some children with LKS have a genetic variant called GRIN2A. This may affect how brain cells communicate. This gene also links to other conditions in the same category as LKS.
Not every child with a GRIN2A gene change develops LKS, so more research is needed to fully understand the connection.
Some children with this syndrome may have changes in other genes, too. These may include:
These changes affect how their brain works during development, sleep and speech.
Researchers are also studying whether there’s a link between LKS and the immune system. An autoimmune disease happens when your immune system damages your body instead of protecting it. Autoimmune damage in your child’s brain or nerves may contribute to LKS. But experts haven’t been able to prove this yet.
A healthcare provider will compare your child’s growth to typical childhood development milestones. Kids with this condition usually meet growth and development guidelines before symptoms start. They could fall behind expected milestones once symptoms begin.
LKS can be tricky to diagnose because it can cause symptoms that might be hard to notice. You may be more likely to pick up on changes because you’re around them every day. Tell your child’s provider if you’ve noticed any new or different symptoms or changes.
Your child’s provider will use a few different tests to diagnose LKS. They’ll probably recommend an EEG. This painless test will show any unusual brain activity that is more prominent when your child falls asleep.
Some tests can help rule out other, more common issues that cause similar symptoms. Their provider might suggest the following:
Providers now group LKS under a condition called EE-SWAS based on your child’s symptoms and test results. If your child had normal development before symptoms began, this helps their provider decide how to classify their condition. This new naming system guides treatment options.
Advertisement
Your child’s provider will suggest treatments to manage Landau-Kleffner syndrome symptoms. Some of the most common treatments include:
There’s no one right way to treat LKS. Your child may improve with speech therapy and other treatments. But they may not respond to treatment. Your healthcare provider will check your child’s progress and adjust their treatment as necessary.
Visit a healthcare provider if you notice any changes in their physical or mental health. You know your child better than anyone. Tell their provider if you’ve noticed any changes in their emotions, behavior or habits.
Whether it’s Landau-Kleffner syndrome or another issue, it’s always best to get noticeable symptoms checked out right away.
You might want to ask your child’s provider a few questions, including:
Advertisement
There’s no quick cure, but some children regain their ability to speak and understand language. Others may only partially recover these skills.
Providers now recognize that LKS can look different for everyone who has it. Some children had normal speech development before symptoms began, while others had speech delays early on. Understanding where your child falls in this spectrum helps your provider plan the most effective care.
It can take a long time for your child to recover. You’ll probably notice slow, gradual improvements in their language skills.
It’s possible that your child may lose language skills after making some progress (a relapse). This is a normal part of treatment, but let your provider know if symptoms come back. They might suggest special education classes or learning sign language to help meet your child’s needs.
No, LKS isn’t a type of autism. Autism is a difference in how your child’s brain works. It may affect how they behave and socialize compared to what people usually expect.
But these conditions can share symptoms, so it can be hard to tell them apart. Often, an EEG taken when your child is awake compared to one when they’re asleep can distinguish between the two conditions. However, it’s possible to have both LKS and autism.
Advertisement
Talk to your child’s healthcare provider if you notice any changes in how they act or communicate. Your provider will help you understand what your child needs.
Watching your child grow and learn new skills is one of the best parts of being a parent or caregiver. If they have Landau-Kleffner syndrome (LKS), it might feel like something is taking that joy away from you both. LKS makes it hard for your child to use and understand language. This can be scary and frustrating. But treatments can help.
Visit a healthcare provider as soon as you notice any changes in your child’s behavior, mental or physical health. The sooner your child gets an LKS diagnosis and starts treatment, the better. Don’t hesitate to ask your provider lots of questions. They’ll help you understand what’s causing the LKS, what you can expect, and how you can help your child now and in the future.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
