Laryngomalacia is a voice box disorder common in newborns. The tissues above their voice box soften and fall over their airway. This causes stridor (noisy or high-pitched breathing). Laryngomalacia usually goes away on its own by the time your baby is 1 to 2 years old. Your healthcare provider can help you manage symptoms in the meantime.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
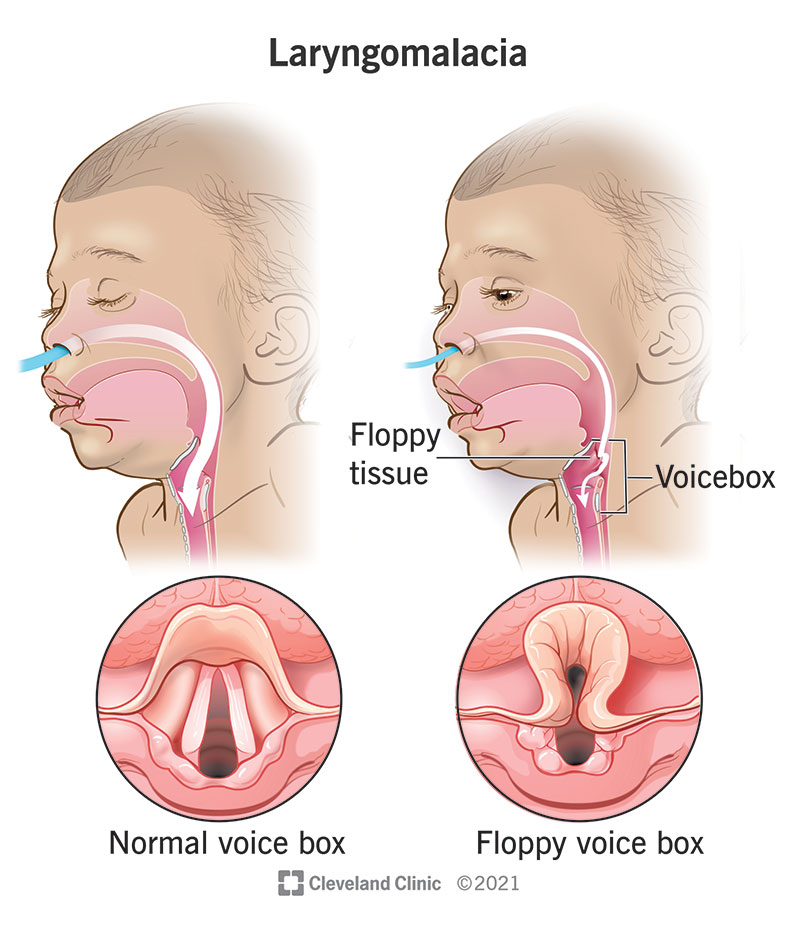
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/22076-laryngomalacia)
Laryngomalacia (lah-ring-oh-ma-LAY-shia) is a larynx (voice box) abnormality that can happen in newborn babies. It occurs when weak, floppy tissues above the voice box temporarily fall back over the airway. It’s the most common cause of noisy breathing in babies.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Laryngomalacia sounds like a high-pitched squeak (stridor) when your baby breathes in. It usually isn’t serious. But in severe cases, it can cause breathing and feeding issues, among other complications.
Congenital laryngomalacia (meaning you’re born with it) is common in infants. Over half of all newborn babies have it during the first week of life, and even more develop it when they’re 2 to 4 weeks old.
Laryngomalacia can also occur in adults, but it’s rare. (Healthcare providers refer to this as acquired laryngomalacia.)
Laryngomalacia symptoms can range from mild to severe. Loud, noisy or squeaky breathing is the main thing to watch for. This often worsens over the first several months but resolves within a year or two.
Most babies with laryngomalacia have no trouble breathing or feeding, even when their breathing sounds concerning. Breathing usually gets louder when lying down, sleeping, crying or feeding.
Babies with severe laryngomalacia may have these symptoms:
Advertisement
If your baby shows any of the symptoms listed above, call their pediatrician right away.
Experts aren’t exactly sure why some babies develop laryngomalacia and others don’t. But they have a few theories about why it happens, in general:
Healthcare providers categorize laryngomalacia into three types according to cause:
Nasopharyngolaryngoscopy (NPL) is the main test healthcare providers use to diagnose laryngomalacia. An otolaryngologist (ENT) uses a scope with a tiny camera (endoscopy) to view your baby’s voice box. They’ll gently guide the scope into your baby’s nostril and down their throat. Providers can do this routine test in about two to five minutes.
If your baby has laryngomalacia, their provider may need to run other tests to determine the extent of the condition. These tests may include:
Most of the time, laryngomalacia goes away on its own within a year or two and the noisy breathing improves over time. In mild cases, you can manage your baby’s symptoms at home. But if your baby has severe laryngomalacia, they might need medication or surgery.
Advertisement
If your baby has mild symptoms, you can usually keep an eye on things at home. Laryngomalacia management depends on your baby’s unique situation:
Ask your provider about specific ways to manage your baby’s laryngomalacia symptoms.
When GERD occurs with laryngomalacia, your baby’s provider may prescribe an anti-reflux medication like a proton pump inhibitor (PPI) or H2 blocker. GERD can worsen swelling associated with laryngomalacia, so it’s important to keep reflux in check if it’s a contributing factor.
Laryngomalacia surgery involves trimming the weak, floppy tissue above your baby’s voice box. This procedure is a supraglottoplasty. An ENT surgeon will do a supraglottoplasty in an operating room while your child is under general anesthesia. Your baby will typically stay overnight in the hospital for observation.
Advertisement
Anti-reflux medication usually improves symptoms within two weeks. But your baby will probably need to stay on the medication for several weeks or months.
If your baby had laryngomalacia surgery, their breathing may sound worse for a few days. This is normal. It’s due to post-op inflammation (swelling) around their vocal cords. The noisy breathing should gradually improve, with full recovery taking about two weeks.
Despite the noisy breathing, laryngomalacia is usually not dangerous. While most babies outgrow laryngomalacia, a few will need surgery to correct the issue, especially if they’re having trouble gaining weight or are having severe breathing difficulties. Your healthcare provider can tell you what to expect if your baby receives a diagnosis.
Laryngomalacia usually goes away on its own by age 1 or 2. But you should keep an eye out for severe symptoms like apnea and a bluish color around their lips. These things can cause serious complications.
You can’t prevent laryngomalacia. But you can manage your baby’s symptoms with treatment.
As a parent, you want to shield your baby from all harm. But laryngomalacia is just something that happens. It doesn’t mean you’ve done something wrong. Although the sounds your child makes may be scary at first, treatment may not be necessary.
Advertisement
If your baby shows symptoms of laryngomalacia, like noisy breathing, consider scheduling an appointment with your healthcare provider. They can examine your baby and make recommendations for referral to ENT, home care and management.
Call your provider right away if your baby develops sudden symptoms, or if they have GERD.
Head to the nearest emergency room if your baby:
Both laryngomalacia and tracheomalacia are conditions affecting the airway. While laryngomalacia refers to floppy tissues above the voice box, the characteristics of tracheomalacia include floppy or weak cartilage of the windpipe, which is below the voice box. Tracheomalacia is far less common — and usually more serious — than laryngomalacia.
Not usually. In fact, babies with severe laryngomalacia may struggle to gain weight.
Lying on their back could make your baby’s laryngomalacia symptoms worse. If you notice that your baby is having difficulty breathing when sleeping on their back, please see your healthcare provider.
Additionally, GERD — which is common in babies with laryngomalacia — may make their symptoms worse.
Laryngomalacia can be concerning, especially if you’re a new parent. Your baby’s high-pitched, noisy breathing might stress you out and make you wonder if there’s something more serious going on. In most cases, laryngomalacia isn’t dangerous. But it’s always a good idea to schedule a visit with your baby’s pediatrician and ask for a referral to ENT if you have concerns.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
You don’t have to live with voice box problems. Cleveland Clinic has the larynx disorder treatments you need.
