Tracheobronchomalacia (TBM) happens when your trachea (airway or windpipe) and bronchial tubes (airways leading to your lungs) close down or collapse, so you have trouble breathing. Babies, children and adults may have TBM. Symptoms include difficulty breathing, wheezing or a barking dry cough. Surgery and other treatments help with symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
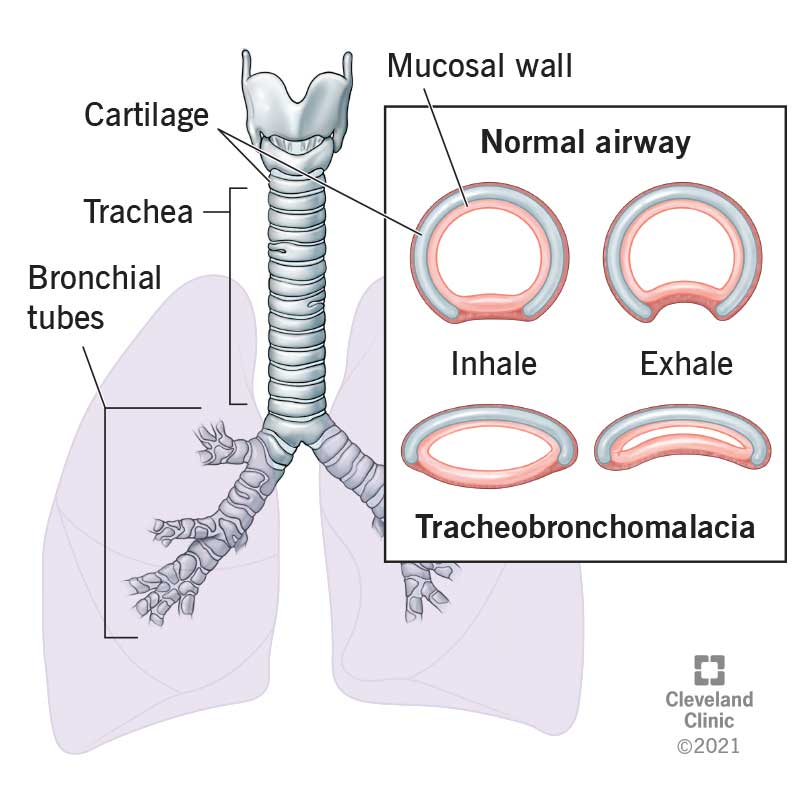
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/22061-tracheobronchomalacia-illustration)
Tracheobronchomalacia (TRAY-key-oh-bronco-mă-LAY-cia) is a condition where your trachea (windpipe) and your bronchi (the tubes that lead from your trachea to your lungs) are so weak that they collapse and close down when you take a breath or cough. If you have TBM, you may have issues breathing. You may wheeze or cough a lot.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Some people are born with tracheobronchomalacia. This is primary or congenital TBM. But you can also develop it during your lifetime. Healthcare providers may call this secondary or acquired tracheobronchomalacia.
Healthcare providers have treatments to help you manage tracheobronchomalacia symptoms. In some cases, they can do surgery to support your trachea and bronchi.
Based on one study, experts estimate 1 in 2,100 babies are born with tracheobronchomalacia. In other research, experts estimate between 4% and 13% of people with airway problems have TBM. But that’s just an estimate, as providers don’t always make the connection between common respiratory problems and collapsing airways.
Symptoms may be different depending on whether you’re born with the condition or develop it over time.
Babies born with TBM may have symptoms that start when they’re 2 to 4 months old. Symptoms may include:
Tracheomalacia symptoms in adults may develop over time and get progressively worse. Symptoms include:
Advertisement
Tracheobronchomalacia happens when the walls of your trachea and bronchi are weak and collapse when you take a breath. Your trachea is a stiff, flexible tube made of cartilage that carries air in and out of your lungs. Your bronchi move air into your lungs and are lined with tiny hair cells that help move mucus and particles out of your lungs.
Primary/congenital tracheobronchomalacia in babies may happen for no known reason (idiopathic TBM). But it may happen if they’re born with conditions, including:
Several things may cause secondary/acquired tracheobronchomalacia including:
Adults with tracheobronchomalacia often have the following conditions that can lead to TBM:
Some medical treatments may cause tracheobronchomalacia:
Exposure to the following toxins may increase your risk of TBM:
A healthcare provider will do a physical examination. If they’re treating your child, they’ll ask you about their symptoms, their overall health and any medical conditions that may be the reason why your child is coughing, wheezing or has trouble breathing.
Advertisement
If you’re having symptoms, your provider will do a physical examination and ask the same sorts of questions. They may ask if you have frequent respiratory infections or other conditions that affect how you breathe.
They may do the following tests:
Treatments vary depending on how tracheobronchomalacia affects your or your baby’s ability to breathe. For example:
Several kinds of supportive devices or durable medical equipment treat TBM symptoms. These devices can help you or your child manage symptoms and limit how much tracheobronchomalacia affects your quality of life. Treatments include:
Advertisement
There are several surgical treatments for TBM. They include:
Tracheobronchoplasty and tracheopexy are major surgeries. Like most surgeries, there may be complications, including:
Advertisement
If your healthcare provider recommends surgery to treat TBM, they’ll explain the risk of complications.
Your child’s trachea cartilage will become stiffer as they grow up. That means there’s less chance that their trachea and bronchi will collapse and affect their breathing. But often, children with TBM need ongoing medical treatment and support to help them breathe.
Sometimes, losing weight or treatment may help with TBM symptoms. But TBM in adults is often a chronic (continuing) condition. If you have tracheobronchomalacia, you’ll probably work with a healthcare provider who specializes in airway treatment for the rest of your life.
Studies suggest that surgery helps ease tracheobronchomalacia symptoms right away and for several years after surgery. If you’re like many people with tracheobronchomalacia, you have other medical conditions that affect your overall health. Those conditions can make it more difficult for you to respond to treatment or recover from surgery.
People who develop TBM often have other serious medical conditions that may affect their life expectancy. Your healthcare provider is your best source if you want to know if having tracheobronchomalacia could affect how long you’ll live.
TBM in adults can be life-threatening because it doesn’t go away and gets worse over time. TBM in babies may cause less serious symptoms as they grow up.
There’s no way to prevent congenital tracheobronchomalacia in children. Adults can develop TBM over time if they have certain medical conditions or have exposure to secondhand smoke or toxic gases.
Tracheobronchomalacia gets worse over time, so talk to a healthcare provider if you know you have exposure to secondhand smoke, toxic gases or conditions that may increase your risk. You may not be able to keep TBM from happening, but there may be ways to keep it from getting worse.
Most children with tracheobronchomalacia will need medical support throughout childhood. For example, you or your child will need treatment like taking medications or using devices that keep your airway clear.
Your child’s pediatrician may schedule regular follow-up appointments to check on your child’s overall health. You may want to ask your child’s pediatrician about ways to protect your child’s overall health, like ways to avoid respiratory infections.
If you have tracheobronchomalacia, here are some suggestions that may be helpful:
If you have TBM, you’ll have ongoing medical care and regular medical checkups. Contact your provider if you notice your symptoms like coughing or wheezing get worse.
You may be surprised to learn issues with your trachea and bronchial tubes are why you or your child has trouble breathing or a barking cough that doesn’t go away. If you or your child receives a TBM diagnosis, you’ll probably want to learn more about it. Here are some questions to get you started:
Tracheobronchomalacia (TBM) can literally take your breath away. If your baby has it, they may struggle to breathe while you breastfeed them. If you have it, you need to stop and catch your breath to finish climbing the stairs. Fortunately, there are many ways to treat TBM and improve breathing. But even with treatment, chances are you’ll need ongoing medical support for the rest of your life. You might be feeling overwhelmed by the prospect of managing a long-term condition. If you are, talk to your healthcare provider. They understand all the special challenges a long-term condition brings and can recommend programs and resources that will help you now and in the future.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Breathing issues can affect your life in many ways. Cleveland Clinic’s respiratory therapy program treats your symptoms so you can feel better day to day.
