Ovarian endometriomas, or “chocolate cysts,” are cysts filled with old blood. They’re a sign of endometriosis, a condition that happens when endometrial-like tissue travels outside of your uterus. These cysts can cause unpleasant symptoms that your provider can help you manage. In some cases, removing them is the best option.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
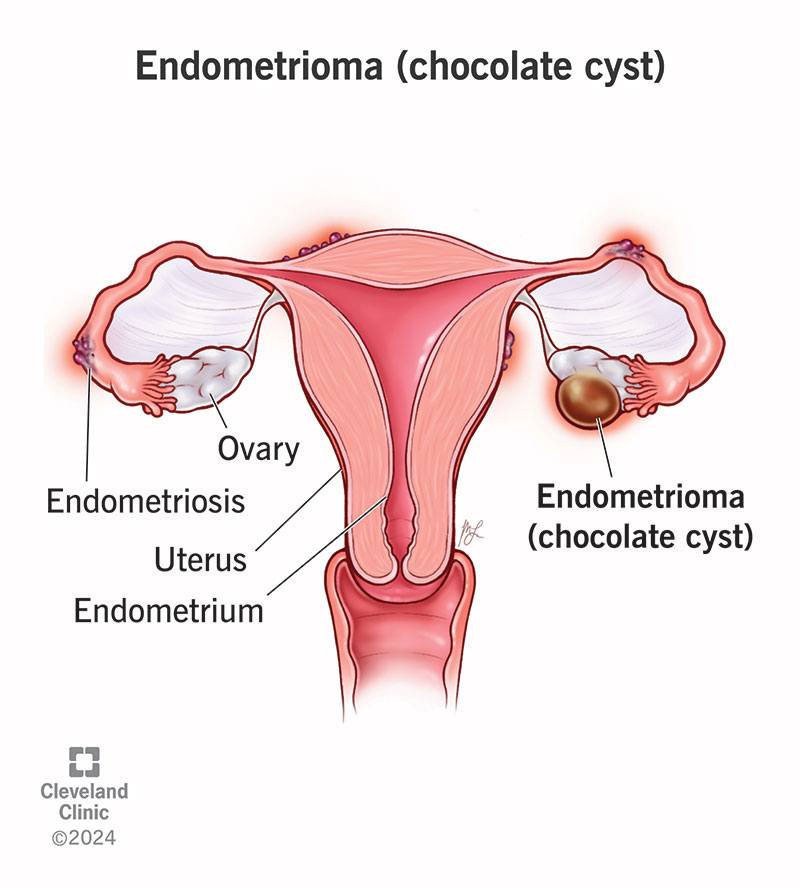
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22004-ovarian-endometrioma)
Endometriosis is a condition where tissue that’s similar to the tissue that grows inside your uterus is growing outside your uterus. It can cause painful periods, pelvic pain and impact your ability to get pregnant. When this tissue attaches to your ovary, it’s called an endometrioma and can be filled with brown, chocolate-like fluid. An endometrioma can cause irritation and attach to other organs. If you have an endometrioma, it can be a sign that you have a more severe form of endometriosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If the endometrioma causes you pain, becomes large or affects your fertility, there are treatments available to help you.
About 10% of people who menstruate have endometriosis, and about 17% to 44% of those people develop ovarian endometriomas.
Pain or tenderness in your pelvis is the most common symptom of an ovarian endometrioma. This pain can happen at any time and not just when you’re on your period. You may notice other symptoms, too, such as:
They can be very small, grow very large and can involve one or both ovaries.
It’s not known what exactly causes an endometrioma. One theory is that endometriosis happens because some of the endometrial-like tissue that you shed when your menstruate flows backward (retrograde menstruation). Instead of leaving your body through your vagina, some of the tissue travels back through your fallopian tubes and onto your ovaries. This tissue thickens and bleeds during each menstrual cycle, leading to inflammation and the formation of an endometrioma cyst.
Endometriomas are a type of endometriosis. Anyone who menstruates can get endometriosis. Some of the risk factors for endometriosis are:
Advertisement
In most cases, endometriomas are signs of a more advanced stage of endometriosis. Other than severe pelvic pain, some of the complications of ovarian endometriomas are:
With a rupture, you’re likely to also have a fever, severe abdominal pain, weakness and other symptoms.
Ovarian endometriomas can become cancerous, but this is rare. Your provider may monitor your cysts and discuss treatment options if there’s concern that an ovarian endometrioma could become cancerous.
Physical exams and imaging procedures can help diagnose an ovarian endometrioma. If the cyst is especially large, your provider may notice it during a pelvic exam. A transvaginal ultrasound or MRI will provide more information.
To officially diagnose an ovarian endometrioma, a surgeon removes the cyst and sends it to a lab for examination. Usually, this happens during a laparoscopy. During this procedure, your provider makes tiny cuts in your abdomen and inserts a camera tube called a laparoscope. Using this tube, your surgeon can see the cyst, remove a sample of it for testing (biopsy) or remove it entirely. The sample is sent to a lab where a pathologist examines it.
A provider may order other tests to rule out conditions that may be causing your symptoms. Your provider may order:
There isn’t a cure for ovarian endometriomas, but a surgeon can remove them if they cause unpleasant symptoms or pose risks to your health. Treatment options include:
Advertisement
The best treatment for you depends on lots of factors, like your age, your symptoms and your plans for becoming pregnant. Weigh the pros and cons of your options with your provider to decide the best plan for you.
You don’t always have to remove an endometrioma. Ovarian endometriomas that are small and don’t cause pain may not need treatment. In this case, your provider may recommend monitoring the cyst over time.
Yes, they can come back even after treatment. The rate of recurrence varies depending on factors like the size of the original endometrioma, your age and the type of treatment you had. About 1 in 4 people will see an endometrioma return.
Advertisement
Having ovarian endometriomas means that you have moderate to severe endometriosis. You should work with your provider to manage any symptoms you’re experiencing because of endometriosis. For example, you may need help managing pain or need to seek treatment for fertility issues (if you’re trying to get pregnant).
There’s no way to prevent an ovarian endometrioma from forming.
Contact a healthcare provider if you have pelvic pain or other symptoms of an ovarian endometrioma. They can perform an exam and order tests to see if an ovarian endometrioma is the source of your painful symptoms.
You should seek emergency care if you have an ovarian endometrioma that bursts. Pay attention to these warning signs:
The differences between the two conditions are what’s inside the cyst and what causes the cyst. In the case of an endometrioma, the cyst contains old blood. An ovarian cyst can contain blood, tissue and other types of clear, brown or red fluid. The other difference is that an ovarian endometrioma is unique and specific to endometriosis. Ovarian cysts can develop for many different reasons other than endometriosis.
Advertisement
One isn’t necessarily worse than the other. Endometriomas are a type of endometriosis. Having endometriomas usually means you have a severe form of endometriosis.
If you have endometriosis, then you know that it can be very painful and disruptive to your life. Developing an ovarian endometrioma on top of that can be even more upsetting. And knowing that painful symptoms usually get better after menopause isn’t comforting, especially if you’re trying to start a family. If you have an ovarian endometrioma, talk to your provider about the treatment options available to you. Your provider can recommend ways to relieve your uncomfortable symptoms.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Endometriosis symptoms can interrupt your life. At Cleveland Clinic, our experts create a treatment plan that matches your lifestyle and goals.
