Alcohol-induced cardiomyopathy is a condition where your heart changes shape because of long-term heavy alcohol use. The changes to your heart’s shape cause long-term damage, leading to heart failure and severe problems. Abstaining from alcohol may help some people recover, but others will need medication or even surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
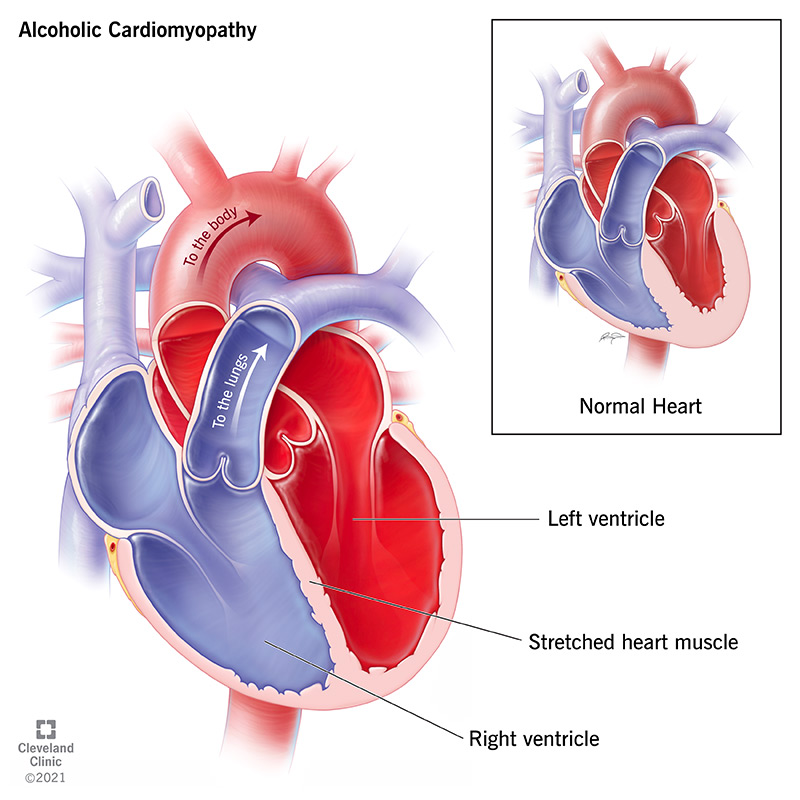
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21994-alcoholic-cardiomyopathy-illustration)
Alcohol-induced cardiomyopathy is a condition where consuming too much alcohol damages your heart. This damage happens because parts of your heart stretch and enlarge. That weakens your heart muscle, keeping it from pumping as well as it should. Over time, this means your heart can't pump blood as effectively, which reduces your body's available oxygen supply.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Alcohol-induced cardiomyopathy can affect anyone who consumes too much alcohol, even those who don't have alcohol use disorder. However, it’s more likely to happen in people with alcohol use disorders or who have genetic mutations that cause them to process alcohol more slowly.
Alcohol-induced cardiomyopathy is a relatively uncommon condition, occurring in about 1% to 2% of people who consume more than the recommended amounts of alcohol.
The available research shows that if you limit your alcohol intake to a certain amount, you’re less likely to develop alcohol-related health problems, including alcohol-induced cardiomyopathy. For women, that amount is seven drinks per week. For men, it’s 14 drinks per week.
The Centers for Disease Control and Prevention (CDC) defines heavy alcohol use — also known as heavy drinking — as more than eight drinks per week for women and more than 15 drinks per week for men. One drink is equal to 14 grams of pure alcohol, which can take many different forms because some forms have a higher concentration of alcohol than others.
Each of the following examples of those forms is equal to one drink.
| Beer | Malt Liquor | Wine | Liquor (Bourbon, Gin, Rum, Tequila, Vodka, Whiskey) |
|---|---|---|---|
| 5% alcohol by volume (ABV) | 7% ABV | 12% ABV | 40% ABV |
| 12 fluid ounces | 8 to 9 fluid ounces | 5 fluid ounces | 1.5 fluid ounces |
| Beer | |||
| 5% alcohol by volume (ABV) | |||
| Malt Liquor | |||
| 7% ABV | |||
| Wine | |||
| 12% ABV | |||
| Liquor (Bourbon, Gin, Rum, Tequila, Vodka, Whiskey) | |||
| 40% ABV | |||
| 12 fluid ounces | |||
| Malt Liquor | |||
| 8 to 9 fluid ounces | |||
| Wine | |||
| 5 fluid ounces | |||
| Liquor (Bourbon, Gin, Rum, Tequila, Vodka, Whiskey) | |||
| 1.5 fluid ounces |
Alcohol-related cardiomyopathy is a type of dilated cardiomyopathy, which is when your heart’s shape changes because its muscles are stretching too much. As the muscles stretch more and more, they also weaken. The effect is much like how a rubber band or spring weakens when stretched too much.
Advertisement
The muscles that control the lower chambers of your heart, the left and right ventricle, are especially prone to this kind of stretching. These chambers are important as they do the majority of the work of your heart, with the right ventricle pumping blood to your lungs and the left ventricle pumping blood to your entire body. Weakening in the muscles around the ventricles means they can’t pump as hard, which negatively affects your entire body.
Changes in your heart’s shape can also disrupt that organ’s electrical system. An electrical current travels through your entire heart with every heartbeat, causing each part of the heart to squeeze in a specific sequence. Your heart’s shape is part of how that timing works, and when parts of your heart stretch, it can disrupt that timing. If it takes too long — even by tiny fractions of a second— that delay can cause your heart to beat out of sync (a problem called dyssynchrony). Similarly, alcohol can have a toxic effect on your heart and cause scar tissue to form. That scar tissue can also cause potentially life-threatening arrhythmias (irregular heart rhythms).
While the long-term effects of alcohol-induced cardiomyopathy tend to get the most attention, there’s also the potential for acute (short-term) problems. An example of this is a condition sometimes known as “holiday heart syndrome.”
Drinking a large quantity of alcohol in a short period can also have toxic effects on your heart muscle. This can cause a disruption in your heart rhythm called “fibrillation.” This is when the chambers of your heart try to beat so quickly that they only twitch or quiver. When chambers of your heart do this, they don’t pump effectively. This happens in one of two ways:
Many of the symptoms connected to alcohol-induced cardiomyopathy happen because of how the condition changes the structure of your heart. Symptoms include:
Advertisement
Alcohol has toxic effects, but your body can limit the damage and break alcohol down into non-toxic forms if you don’t drink too much too quickly. However, consistent heavy drinking strains those protective processes — especially in your liver — making them less effective. Ultimately, your body can’t keep up with the damage to multiple organ systems, including your heart.
While alcohol-induced cardiomyopathy comes from long-term alcohol abuse, there’s no universal limit or number that means you’ll develop it. However, researchers have pinpointed certain behaviors that make it more likely you’ll develop this condition.
Advertisement
Though they aren't causes of alcohol-induced cardiomyopathy, other lifestyle choices can make it worse. These include using recreational drugs (especially those that affect your heart, such as cocaine) and tobacco (which has major negative effects on your heart, lungs and circulatory system).
A doctor can diagnose alcohol-induced cardiomyopathy based on a combination of diagnostic tests, your medical history and by asking you questions about your lifestyle and personal circumstances. A medical provider uses those means because they need to confirm the following:
Advertisement
To diagnose this condition, healthcare providers will typically use several of the following methods.
This involves a doctor examining you for visible symptoms such as swelling in your legs or bulging neck veins. They will also use a stethoscope to listen to your heart and lung sounds. Alcohol-induced cardiomyopathy commonly causes a crackling sound in the lungs and heart murmurs (an unusual sound in your heartbeat that can indicate a problem).
To diagnose changes in the shape of your heart, doctors need to see the shape of your heart in the first place. They can do that using the following tests:
Some of the above tests may also use materials injected into your bloodstream that are highly visible on certain types of imaging scans. Those materials, such as contrasts or tracers, are helpful because they can reveal blood flow blockages that would be very hard to see otherwise.
Treatment for this condition starts with helping you reduce your alcohol intake or stop drinking entirely. That also may involve supportive care that will help prevent — or at least reduce the impact of — any alcohol withdrawal symptoms. Supportive care for withdrawal is especially important because some of its symptoms can be severe or even life-threatening. A healthcare provider can also connect you with available resources and refer you to other specialists and experts who can help you reduce or stop your alcohol intake.
In many — if not most — cases, abstaining from alcohol can be enough to help people recover from alcohol-induced cardiomyopathy. In cases where people don’t recover fully by abstaining from alcohol, most people will still see noticeable improvements in their symptoms. In some cases, even just reducing alcohol intake to light or moderate levels can also lead to improvements. However, not drinking at all is still the best course of action whenever possible.
As you reduce your alcohol intake, your provider will also treat your symptoms. This usually involves certain types of medications that treat heart rhythm problems or other symptoms of heart failure. Those who don’t fully recover are also likely to need this kind of treatment indefinitely. In some cases, a pacemaker or other implantable device might be necessary to treat more severe heart rhythm problems. Others might need surgery to repair damage to the heart’s valves.
The only way to cure alcohol-induced cardiomyopathy is with a heart transplant. However, this is usually not an option because there are so few hearts available from organ donors. For that reason, transplant programs have very strict list requirements to qualify for a transplant and abstaining from alcohol is almost always on those lists.
Completely abstaining from alcohol is the key recommendation if you have alcohol-induced cardiomyopathy. Your healthcare provider will likely recommend that you also focus on improving your diet in ways that help your heart. This usually involves limiting your sodium (salt) and cholesterol intake and ensuring you are getting a diet that provides all essential nutrients. That’s because vitamin and mineral deficiencies are more common in individuals who are chronic heavy drinkers. Consider a heart-healthy diet, such as the Mediterranean diet or the DASH diet.
Many medications can help in cases of alcohol-induced cardiomyopathy, treating the symptoms that happen because of this condition. Medications typically include beta-blockers (for heart rhythm and blood pressure issues) and diuretics (to help your body get rid of excess fluid and swelling).
In some cases, especially those that are more severe, heart failure symptoms and related conditions may develop or get worse. Your healthcare provider is the best person to explain the risks and possible complications that you might face from this condition itself, related health concerns or any of the treatments that you will receive.
In general, most people who stop drinking alcohol will feel better over the next three to six months. However, certain symptoms may start to improve even sooner, depending on treatments and the severity of your case. In more severe or complicated cases, especially ones involving surgery, some symptoms may not improve for even longer. Overall, your healthcare provider is the best source of information and answers when it comes to your recovery.
What you should expect with this condition depends strongly on several factors. One of the biggest factors is your history with alcohol. This condition tends to be worse the more you drink and/or the longer you were a heavy drinker. Other health problems you have can also affect your case, especially if those problems have any connection with alcohol use.
Your outlook tends to be better if you can stop drinking entirely. However, even reducing your drinking to light or moderate levels is better than continuing to drink heavily. Your outlook may also improve depending on other treatments you receive, such as medication or surgery.
For many people, abstaining from alcohol can lead to a full recovery, especially when your case is less severe. However, for others, the effects of alcohol-induced cardiomyopathy may be life-long. Even in cases where people can undergo a heart transplant, individuals with a history of alcohol-induced cardiomyopathy are more likely to face other health problems down the road.
Alcohol-induced cardiomyopathy, especially when more severe, leads to deadly problems like heart attack, stroke or heart failure. Individuals with this condition who don't stop drinking heavily are at the greatest risk. Between 40% to 80% of people who continue to drink heavily will not survive more than 10 years after receiving this diagnosis.
The best way to reduce your risk of developing alcohol-induced cardiomyopathy is to only drink in moderation. That is especially true if you have any kind of condition that affects how your body processes alcohol.
The only way to completely prevent alcohol-induced cardiomyopathy is not to drink alcohol at all.
The most important thing you can do to help yourself if you have alcohol=induced cardiomyopathy is to quit alcohol if at all possible. If you can't quit, the next best thing is to reduce your drinking to moderate or light levels, and the less alcohol you drink, the better. Moderate drinking means no more than 14 drinks a week for men or 7 drinks a week for women.
You should also follow your doctor’s guidance and advice on any treatments you receive. This includes taking your medication as instructed and eating a healthy diet. If you have any questions about how to do either of these, your healthcare provider can answer them and offer you help and resources along the way.
In general, you should talk to your healthcare provider if you notice changes in your symptoms over time, especially if they are starting to affect your normal life and routine. However, you should talk to your healthcare provider about symptoms that mean you should call their office because each case is different.
Your healthcare provider is the best person to tell you what symptoms mean you need urgent medical care. However, in general, you should go to the emergency room if you have the following symptoms:
Alcohol-induced cardiomyopathy is a condition that can have major impacts on your life over time. While many people will recover from this condition if they abstain from alcohol, others will have symptoms and related problems for the rest of their life. If you are a heavy drinker, talking to a primary care provider can help keep this condition from becoming even more severe in the future, or even prevent it from happening. Your provider is the best source of information and guidance, and they can connect you to other resources that can help and experts who can assist.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic can diagnose and treat heart failure of any kind, at any stage, with advanced therapies and compassionate care.
