Acanthamoeba keratitis is a rare eye infection you can get from an amoeba, a microscopic creature similar to bacteria but a little more complex. People who wear contacts or are immunocompromised have the highest risk of contracting this condition. It’s treatable, but the best way to deal with this condition is to prevent it from happening.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
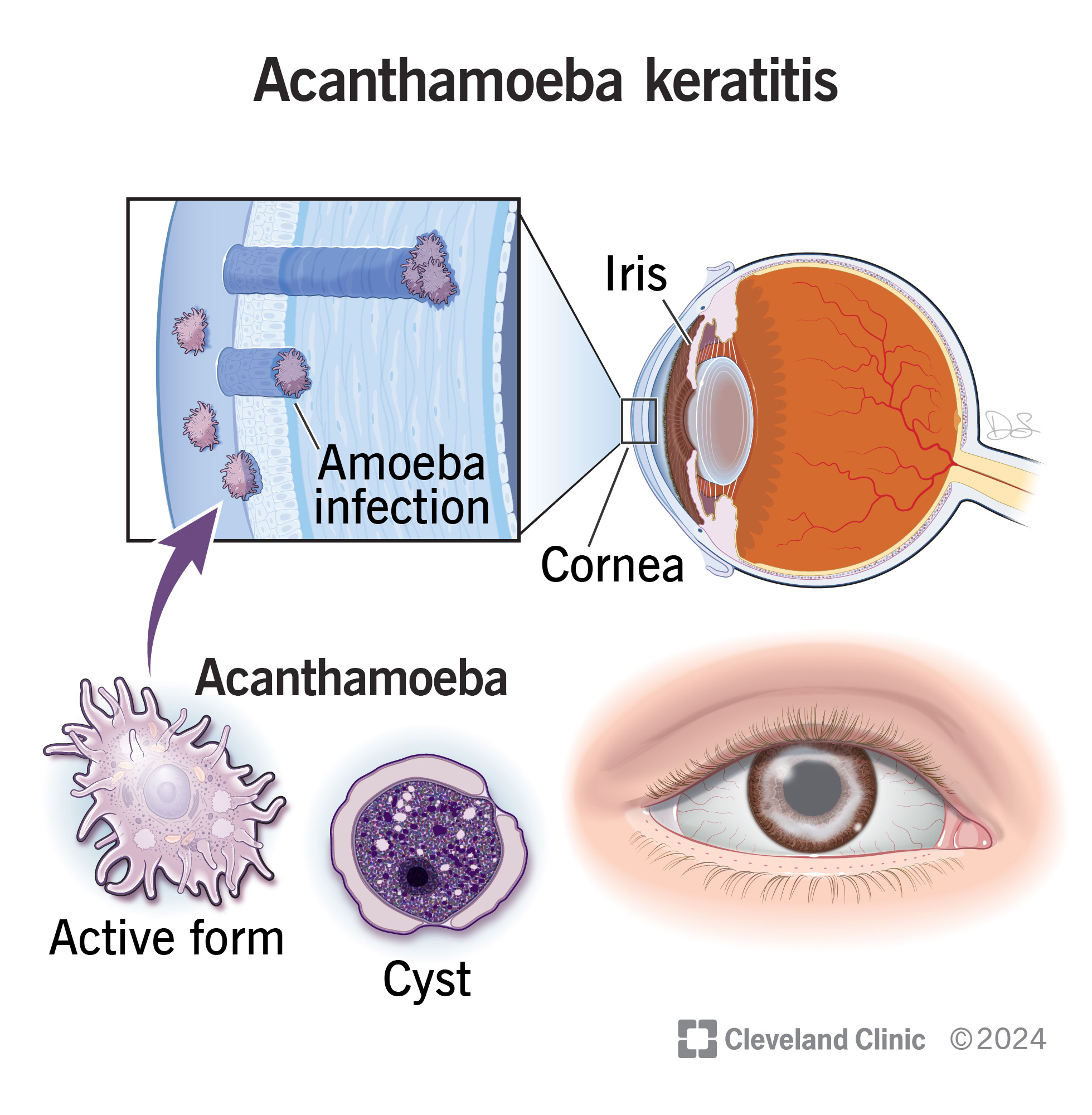
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/acanthamoeba-keratitis)
Acanthamoeba keratitis (AK) is a rare parasitic eye infection from a certain type of amoeba. It affects the cornea, the clear, dome-shaped front covering of your eye. When not treated, it can damage your eyes and cause loss of sight.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This condition is sometimes known as “amoebic keratitis” or by similar names. AK usually affects one eye at a time, but it can affect both. It starts by affecting the outermost layer of your cornea, the epithelium. As it gets worse, the infection extends deeper.
An amoeba is a single-celled organism. It‘s similar to bacteria but a little more complex. It isn‘t a true parasite because it can go through its entire life cycle without needing to infect humans or any other animals. But amoebas act like parasites when they infect humans or animals.
Scientists know of at least 20 species of acanthamoeba worldwide. They can live almost anywhere humans do, and they easily survive in freshwater, seawater, soil and many other places. Researchers know of eight (possibly nine) acanthamoeba species that can cause AK.
During their life cycles, acanthamoeba can take two forms. One is their active, mobile form. The other is their cyst form. This form involves a toughened outer layer. In cyst form, acanthamoeba can survive all kinds of threats that would kill them otherwise.
That includes:
Advertisement
Knowing that is important because acanthamoeba can enter your body both in active and cyst forms. That’s why you should take proper precautions to prevent them from infecting you.
AK is rare overall. Research indicates there could be up to 1,500 cases in the U.S. each year.
The symptoms of AK happen when the active form of these microbes enters the corneas of your eyes. The symptoms may not remain constant, cycling back and forth between better and worse.
Symptoms include:
Two species of acanthamoeba cause most cases of AK (experts abbreviate “acanthamoeba” to “A.” in the species names). The two species are A. castellani and A. polyphaga.
AK is infectious (meaning you can catch it), but it isn’t contagious (you can’t directly catch it from someone else).
The most common ways for acanthamoeba to infect your eyes are:
Contact lens wearers make up at least 90% of AK cases. That’s usually because of a combination of factors. The factors include:
Acanthamoeba can survive in water easily, especially in cyst form. Even treated drinking water, bottled water or swimming pool water may not have a high enough chlorine concentration or other disinfectants. That’s why you should never use tap water with contacts or wear contacts while swimming.
Under ordinary circumstances, acanthamoeba from these sources can’t infect your eyes. But there are times when they can. Some include:
The cornea is like your eye‘s windshield, but injuries make it less effective. The injuries are like weak points or small gaps in the cornea surface where it‘s easier for microbes to get in. Injuries to your corneas usually involve contact lenses, your fingers or fingernails, plants or plant material, or dirt or soil.
Advertisement
There are a few main complications that are possible with AK:
AK is tricky to diagnose early on, and an initial misdiagnosis happens in about 75% to 90% of cases. That’s because of the following:
Your eye care specialist will do an eye exam, including a slit lamp exam. That lets them look into your eyes for signs or clues. They’ll also ask about your symptoms, recent activities or if there could be other contributing factors.
The standard practice is to treat any eye infection as if it were viral or bacterial first and suspect it’s AK if treatment doesn’t work. If it doesn’t, your eye care specialist will likely recommend starting treatment for AK.
Advertisement
Testing for AK may involve taking samples of corneal tissue. That can involve:
Both of these tests are more invasive and can be painful. But your provider will use numbing drops or medications to help with that. Corneas also regenerate quickly, which reduces how long you feel pain or discomfort from a scraping or biopsy.
The wait time for results from corneal tissue testing can take several days. Your provider will likely begin treatment to help with your symptoms in the meantime.
Treating AK has two main goals: getting rid of the infection and reducing pain and other disruptive symptoms. Medications are usually the first option, and surgery may be necessary in more severe cases.
Many of the more common AK medications aren’t available in the United States anymore because the condition is so rare. But some pharmacies may be able to custom-make (compound) these medications for you. Your eye care specialist is the best person to tell you about medication options and where you might be able to get them.
Advertisement
Active forms of acanthamoeba are very sensitive to certain medications. In cyst form, acanthamoeba species can resist treatment, but some medications can still overcome that.
The main form of treatment is topical antiseptic drops, such as chlorhexidine and polihexanide (also known as polyhexamethylene biguanide, or PHMB).
About 40% of AK cases don’t respond well enough to medication alone. When that happens, surgery may be the next best option. This can include:
AK is a condition that can be very painful — often much more than your other symptoms or visible eye changes would suggest — and disruptive. It’s important not to ignore it because it gets harder to treat the longer you wait.
If you have AK, your eye care specialist will first try to treat and/or rule out viral and bacterial infections. Make sure you follow up with them and know how long to wait before contacting them again if treatment doesn‘t seem to be helping.
It’s also important to follow your provider’s treatment instructions exactly as guided. That gives you the best chance of a favorable outcome. If you don‘t follow your provider‘s treatment instructions, you may be prone to reinfection. The cyst form can also live dormant in your corneas for extended periods, which can cause AK symptoms to return months after treatment.
AK can cause severe and permanent damage if it goes untreated for too long. The possible complications include glaucoma, iris atrophy (shrinking or moving out of place), cataracts and chronic defects in the cornea’s outermost layer. In more severe cases, major vision loss is possible.
The outlook for AK depends on several factors. Positive outcomes are much more likely if you get medical care before this condition spreads past the second layer of your cornea. That usually means starting treatment within three weeks of when your symptoms start.
You should see an eye care specialist if you have AK symptoms lasting more than a few days. Doing so will allow them time to try bacterial infection treatments, and if those don‘t work, your eye specialist can have you begin AK-specific treatments.
AK is mostly preventable, though uncommon cases can happen for reasons you can’t control. Steps you can take include:
Yes, AK is curable. This is easier to do when you get treatment sooner rather than later.
AK is rare overall. You’re more likely to get it if you wear contacts and don’t maintain or store them properly. People with decreased immunity also have a higher risk.
No, AK isn’t an emergency condition. But you need to make an appointment and see an eye care specialist as soon as possible.
There’s no way to tell if you have AK (or any other amoeba-related infection) on your own. Only certain medical tests can show it. If you think you might have AK, you need to see an eye care specialist for diagnosis and treatment.
AK is a rare, painful condition that can damage your eyes and cause vision loss if not treated quickly. Fortunately, you can usually avoid this infection with simple precautions. If you wear contacts, make sure you wear, store and maintain your contacts properly. Your eye care specialist can help you if you have questions about how to do this. And if you might have AK (or any other eye infection), don’t try to tough it out. Getting care quickly can treat eye infections and help you feel better sooner.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s ophthalmologists and optometrists have the highest training available. We provide exams, vision correction and care for many eye conditions.
