Plague is an illness you get from Yersinia pestis bacteria. It can infect your lymph nodes (bubonic), blood (septicemic), lungs (pneumonic) or throat (pharyngeal). It most commonly spreads through flea bites. Plague caused deadly outbreaks in the past and still exists in many countries today. Quick antibiotic treatment makes it less deadly now.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
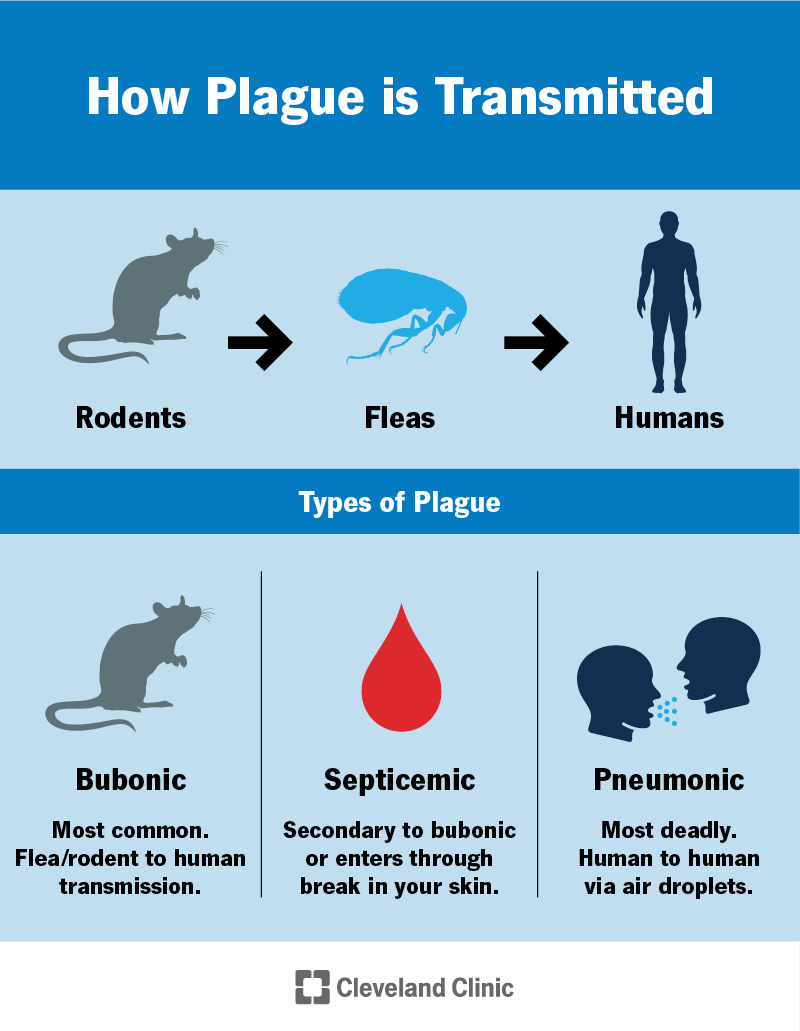
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/plague)
Plague is an illness you get from the bacteria Yersinia pestis (Y. pestis). It usually spreads through flea bites, but you can also get it from other people and animals.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There have been severe outbreaks of plague throughout history. It still exists today, but it’s very rare. Worldwide, 1,000 to 2,000 people are diagnosed with plague every year. Only a few cases are reported in the U.S. each year.
The type of plague you have depends on where in your body you’re infected with Y. pestis:
Some plague symptoms depend on the kind of plague you have. Others happen in all types. Symptoms include:
Advertisement
Yersinia pestis (Y. pestis) bacteria cause plague. Rats, other mammals and fleas can carry Y. pestis. It can spread to people from animals and other people.
You can get plague:
Plague can also move through your bloodstream to different parts of your body (secondary infection).
Plague mostly affects people living in a few countries in Africa. It’s most common in Madagascar and the Democratic Republic of Congo. Cases are also reported in the Americas and Asia every year.
In the U.S., you’re more likely to get plague in rural areas of western states. You’re at a higher risk if you work with animals in an area where plague is found.
Most people think of rats as the only carriers of plague. But many animals carry and spread the disease. Which animals are more likely to have plague depends on where you live. Plague can affect:
Many complications of plague happen quickly and are life-threatening. These include:
To diagnose plague, your healthcare provider will take a sample of your blood, mucus from your lungs or throat, or fluid from a lymph node. They’ll send your sample to a lab to look for signs of Y. pestis.
Make sure to tell your provider if you:
Healthcare providers treat plague with antibiotics. They’ll give you medication either through a vein (IV) or in a pill. Depending on your symptoms and risk, you may start antibiotics even before test results come back. Your provider might also give you extra oxygen or other treatments to manage your symptoms.
Advertisement
You need immediate treatment if you have plague. You have the best chance of getting better if you start treatment within 24 hours of noticing symptoms.
You’ll probably feel better within a week or two of starting treatment. Take any medications as prescribed, even if you feel better. Buboes from bubonic plague might take a few weeks to go away. Ask your provider how long you should avoid other people to prevent spreading the bacteria.
Contact your healthcare provider for immediate medical attention if you:
Yes, you can recover from plague with antibiotics. But you need to be treated right away. The kind of plague you have makes a difference, too. Pneumonic plague is almost always fatal without treatment.
You can reduce your risk of plague by avoiding flea bites and being careful around animals that could be infected. Specific strategies include:
Advertisement
What people sometimes call “the Black Death” was a plague outbreak that killed millions of people in Europe, Asia and North Africa in the mid-1300s. Hunger and poor sanitation made people vulnerable to sickness, and it spread to different countries through trade routes. It’s usually what people mean when they talk about “the plague.”
In the past, millions of people died in plague pandemics. Today, avoiding something “like the plague” means safe animal handling and flea management strategies. It still exists, but thanks to modern sanitation and antibiotics, very few people die from it. But it’s critical that you receive treatment immediately.
See a healthcare provider right away if you think you’ve been exposed to plague and have symptoms.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Have a virus, fungus or bacteria? Some of these “bugs” won’t go away on their own. Cleveland Clinic’s infectious disease experts are here to help.
