Lichen planus is a condition that causes skin inflammation. The resulting rash can affect the skin on your arms, legs, scalp, nails, genital area and the inside of your mouth. For most people, it resolves without treatment. Some treatments can alleviate related symptoms, including itching.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
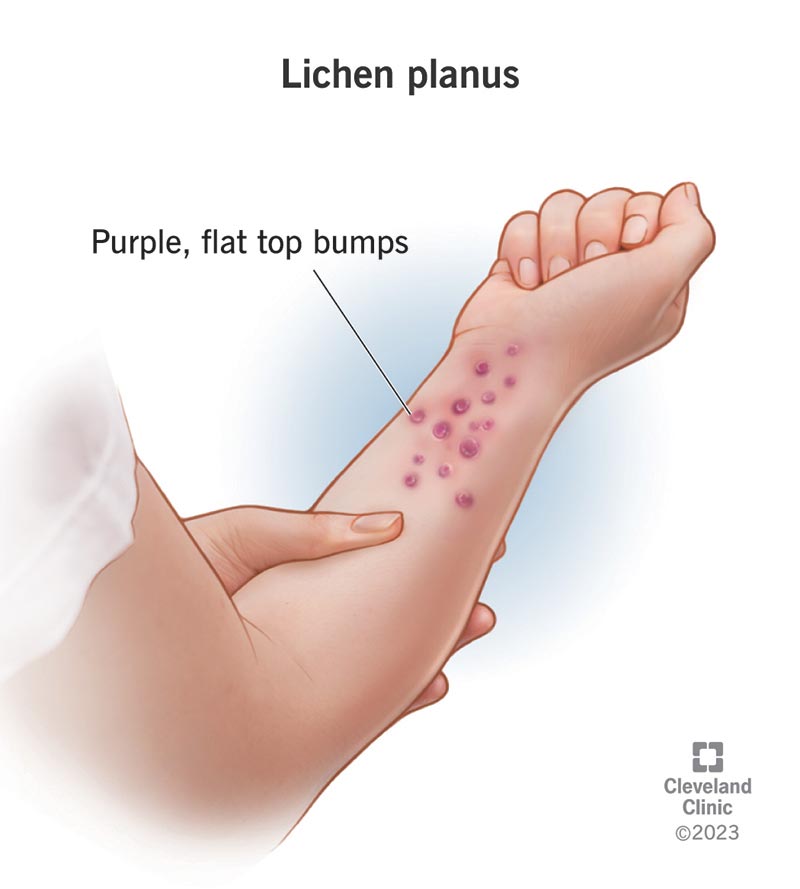
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17723-lichen-planus)
Lichen planus (like-en play-nes) is a skin condition that causes a rash to develop on one area of your body or several parts of your body at the same time. It can affect your:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Lichen planus is a lichenoid dermatoses. Healthcare providers use the term used to characterize skin disorders according to the presence of firm, raised, discolored bumps on your skin.
Lichen planus isn’t an autoimmune condition, but it can cause a similar response. It’s an idiopathic (meaning the cause is unknown) condition that causes inflammation in your skin. In lichen planus, your body’s immune system attacks parts of your body instead of protecting your body from foreign invaders like bacteria or viruses.
In a healthy immune system, special cells in it called T cells help protect your body from infection. In people with lichen planus, their immune system’s T cells attack a protein in their skin and mucus membranes.
No one knows why the T cells attack the protein.
Lichen planus and lichen sclerosus are both idiopathic conditions that affect your skin, especially mucus membranes.
Lichen sclerosus is a long-term skin condition that causes your skin to gradually become thinner, itch, develop sores and eventually scar. It can occur anywhere on your skin, but it mainly affects the skin around your genitals and anus (anogenital region). You're more likely to have it if you've gone through menopause.
Advertisement
The difference between lichen planus and lichen sclerosus is that lichen sclerosus rarely affects the mucous membranes in your mouth.
Lichen planus and psoriasis are both skin conditions that can cause discolored rashes. The main difference between lichen planus and psoriasis is that psoriasis is scaly and typically won’t affect the inside of your mouth.
Anyone can get lichen planus. However, you’re more likely to develop it if you’re a female between 30 and 60 years old.
Some studies suggest that females get lichen planus twice as often as males, and they’re more likely to develop it in their 60s. Males are more likely to develop it in their 40s.
If you have lichen planus on your skin, you’re 50% to 75% more likely to have it in your mouth.
Lichen planus affects approximately 0.22% to 1% of the adult population. Oral lichen planus affects 1% to 4% of the world population.
Lichen planus commonly affects the skin around your wrists and elbows (flexor surfaces), the back of your hands (dorsal surfaces) and the fronts of your lower legs.
About half of all people who have lichen planus develop oral lichen planus, which affects the skin inside of your mouth and your tongue.
The affected spots (lesions) on your body usually start as tiny, raised dots (papules) that are about the size of the tip of a pin (0.4 millimeters [mm]). They may grow up to the width of a pencil (1 centimeter [cm]).
Oral lichen planus typically starts as tiny white dots on the skin inside of your cheeks or your tongue. In severe cases, the surrounding skin may become inflamed, and sores may develop.
Lichen planus symptoms depend on where it’s affecting your body:
Lichen planus doesn’t hurt. However, if you scratch your rash, you may break your skin, leading to an infection that can cause pain.
The following may cause lichen planus flare-ups:
Lichen planus isn’t contagious. You can’t spread lichen planus to another person through unprotected sex or skin-to-skin contact.
Your healthcare provider can typically diagnose lichen planus after assessing your symptoms and conducting a physical exam. They may look for characteristics known as the “six Ps” that help diagnose lichen planus:
Advertisement
If there’s any doubt, your healthcare provider may perform the following tests:
There isn’t a cure for lichen planus. If you have lichen planus on your skin, in most cases, it goes away without treatment in as little as a few months to several years.
The following treatments may help relieve your symptoms:
Advertisement
If you have lichen planus in your mouth, in most cases, it goes away within five years. If you experience irritation or sores, you can help alleviate your symptoms by:
There are several over-the-counter products or home remedies that can help stop your rash from itching.
While home remedies are safe for most people, it’s a good idea to check with your healthcare provider before trying some of the following options. You may be at risk of developing an allergic reaction.
Advertisement
Stress can also make skin disease worse. There are mental/emotional signs of stress and physical signs of stress. Stress management techniques can help you prevent or ease your stress-induced lichen planus symptoms.
Some psychological signs of stress that can make your lichen planus symptoms worse include:
Some physical signs of stress that can make your lichen planus symptoms worse include:
If you have oral lichen planus, it’s a good idea to avoid spicy or acidic foods or drinks that may cause further irritation, including:
In addition to avoiding spicy and acidic foods and drinks, you should avoid smoking.
Lichen planus can be managed without treatment. But most cases will require treatment. If you have lichen planus on your skin, it may take a few months or a few years to go away. If you have oral lichen planus, it may take up to five years to go away. Therapy and home remedies can provide relief if you experience any symptoms.
If you have lichen planus on your penis, vagina or vulva, you may experience discomfort or pain during sex. You can’t give your partner lichen planus through unprotected sex.
There isn’t any way to prevent lichen planus.
Call your healthcare provider if:
Lichen planus is a common skin rash that can also affect your mouth and nails. It can make you feel self-conscious, and it can be unpleasant if it itches. However, it isn’t dangerous or contagious, and it usually goes away on its own.
It’s important to pay attention to your skin. Contact your healthcare provider as soon as you notice a rash.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
