A rectocele is a condition in which weakened muscles in your pelvis cause your rectum to sag against your vaginal wall. It’s a form of pelvic organ prolapse. If the bulge (prolapse) is small, you may not notice symptoms. With a more significant prolapse, you may have difficulty pooping. Healthcare providers typically recommend nonsurgical management first to fix a rectocele.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
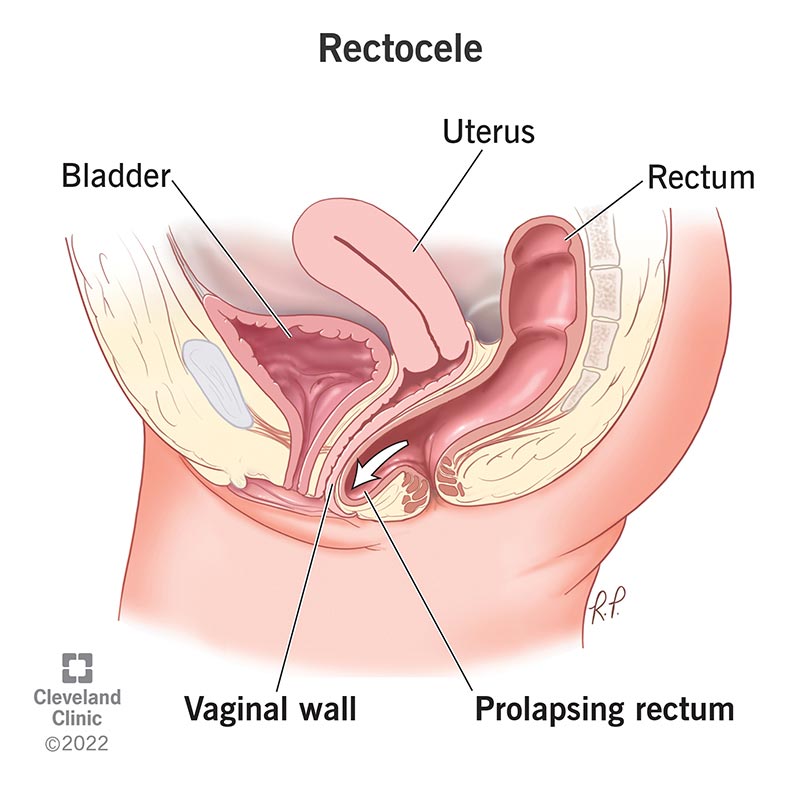
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17415-rectocele)
A rectocele happens when the tissue between your rectum and vagina weakens, causing your rectum to bulge onto your vagina’s back wall. It’s also called posterior vaginal wall prolapse.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your rectum is the bottom part of your colon (large intestine). Your pelvic floor muscles typically keep your rectum and vagina in place. When your pelvic floor weakens, these organs can shift and even fall onto each other.
Rectocele is one form of pelvic organ prolapse (POP). Often, it happens with other forms of POP, like uterine prolapse and fallen bladder.
Rectoceles aren’t life-threatening, but they can decrease your quality of life. Know that you have a few treatment options that can help fix it.
Symptoms of a rectocele include:
Rectoceles don’t always cause symptoms. When they do, they’re usually more unpleasant or uncomfortable than painful. Still, it’s important to talk to your gynecologist or primary care provider if you think you may have a rectocele.
Advertisement
A rectocele happens when your pelvic floor weakens. Several factors can contribute to this. The most significant risk factors include:
Other risk factors include chronic cough or bronchitis and repeated heavy lifting.
Gynecologists can often diagnose a rectocele by asking about your medical history and doing a pelvic exam. In addition to examining your vaginal canal for signs of prolapse, your provider may test your pelvic floor strength during the exam.
They may ask you to squeeze and relax your pelvic floor muscles as if you were stopping a stream of pee. They may also ask that you apply pressure to your gut or strain as if you were pooping. Doing this makes the prolapse more visible.
Your provider may use a grading or staging scale to describe the severity of the rectocele based on the pelvic exam.
In rare cases, your provider may recommend a transvaginal ultrasound to check if your small intestine has prolapsed (enterocele). They may also recommend a special X-ray or an MRI called a defecography. It shows the changes in your rectum when you poop. It can reveal how severe a rectocele is.
Healthcare providers typically recommend nonsurgical management first to fix a rectocele, especially if you have a mild one. For moderate to severe prolapse, your provider may recommend surgery to repair it.
Nonsurgical management strategies include:
If conservative treatment isn’t enough to resolve your symptoms, surgery is the next option. You and your provider will discuss the following to determine the right procedure:
Advertisement
A common surgery for rectoceles is called posterior colporrhaphy. Your surgeon removes damaged tissue that’s no longer supporting your pelvic organs. They suture (stitch) the healthy tissue together for added support.
Often, surgeons perform rectocele surgery through your vagina — an approach that leaves no scars.
If your symptoms get worse or your treatment plan doesn’t seem to be working, let your healthcare provider know.
It may be helpful to ask your provider the following:
Your outlook depends on your symptoms and how severe the prolapse is. Most people who receive surgery for rectocele experience symptom relief after the procedure.
Advertisement
Talk to your healthcare provider about your outlook based on the treatments they recommend for you.
Rectocele may worsen without treatment and lifestyle adjustments. Your symptoms may get worse over time, further impacting your quality of life.
You can’t always prevent a rectocele or pelvic organ prolapse. But many practices can help strengthen your pelvic floor. You can use many of the management strategies for rectocele to reduce your risk of prolapse. This includes regular pelvic floor exercises and avoiding constipation.
Yes. With severe prolapse, poop can become trapped in the pocket of the rectocele. This prevents poop from passing easily.
In this case, you may have to try splinting to pass a stool. Splinting involves putting your finger in your vagina and pressing against the rectocele to nudge the poop out. Ensure that your finger is clean (bacteria-free) before inserting it into your vagina. Wash with mild soap and water.
Talk to your healthcare provider about treatment options if you have to use your fingers to have a bowel movement.
A rectocele is like a hernia, in that your rectum bulges (herniates) into your vaginal wall. But healthcare providers classify rectoceles as a type of pelvic organ prolapse, not a hernia.
Advertisement
Having a rectocele can feel both uncomfortable and embarrassing. Thankfully, treatment can help you regain control over the parts of your body that seem to have a mind of their own. You just have to reach out to a healthcare provider for help. Many people can manage rectoceles through physical therapy and lifestyle changes. If the prolapse is more severe, a provider can recommend surgeries that can help.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
You’ve had your baby, but your care doesn’t end when you leave the hospital. Cleveland Clinic offers expert postpartum care during the fourth trimester.
