Ischemic optic neuropathy (ION) is when you have sudden vision loss or changes because your optic nerves aren’t getting enough blood flow. It’s rare and is most likely to happen in people over 50. Permanent vision loss is possible, so it’s important to get care fast and limit the damage this condition can cause.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
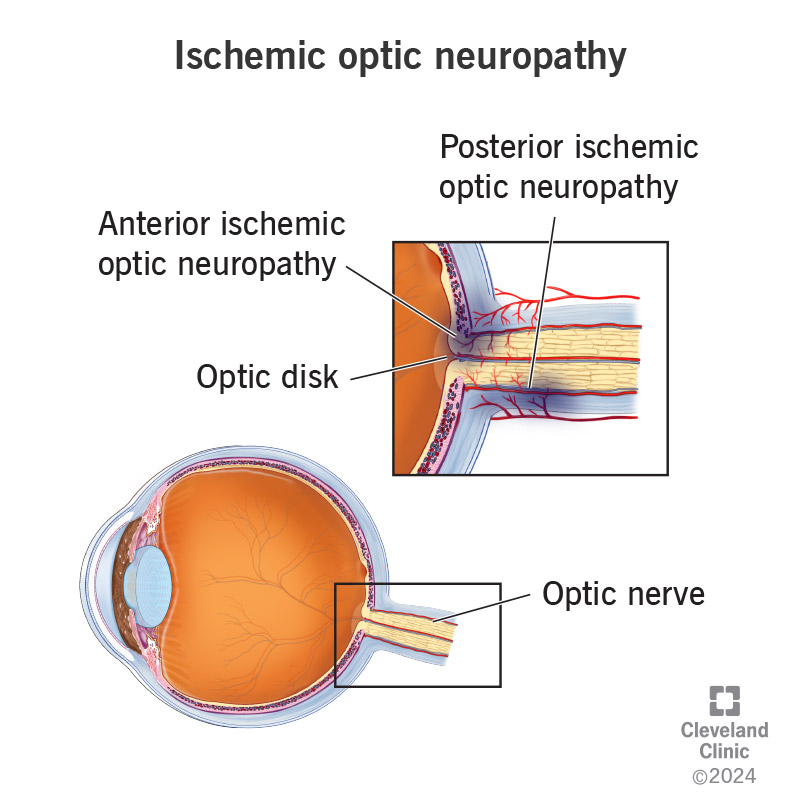
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/ischemic-optic-neuropathy)
Ischemic optic neuropathy (ION) refers to several conditions that all cause vision loss because of a lack of blood flow to part of your optic nerve. Without blood flow, the affected areas stop working correctly and start to die. If the disruption in blood flow is severe or lasts too long, it can damage the optic nerve permanently.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The optic disk at the back of your eye is a circular area where blood vessels and the optic nerve attach to your eye itself. ION happens around the bowl-shaped center of the disk, the optic cup or farther back along the optic nerve. ION isn’t common and generally affects people over age 50.
There are two main types of ischemic optic neuropathy:
This is the most common form of ION. It affects the part of the optic nerve just underneath the optic disk or the optic disk itself. AION has two subtypes: arteritic anterior ischemic neuropathy (AAION) and nonarteritic anterior ischemic neuropathy (NAION).
Arteritic conditions involve arterial inflammation (arteritis). These conditions usually happen with types of vasculitis (blood vessel inflammation). Nonarteritic means there’s no arterial inflammation and it usually happens because of limited blood flow to the optic nerve.
This type of ION happens farther back along the optic nerve. It also has two main subtypes, arteritic and nonarteritic.
The main symptom of ION is vision loss. The way it happens can vary depending on the type of ION. Other symptoms also vary depending on the ION type.
Advertisement
Vision loss from NAION is usually sudden (rapid onset) and painless. It often looks like blurring or worsened vision across part of your field of view (usually in the lower half) in the affected eye(s). It can also cause weakened color vision (dyschromatopsia).
Most people first notice they have vision loss when waking up (either from longer sleep periods or brief naps). Less commonly, vision loss may happen gradually over about two weeks.
NAION, the most common form of ION, usually affects one eye at a time. About 15% of people who have NAION in one eye eventually develop it in their other eye, too.
AAION usually causes sudden vision loss. That means it can cause blurring, darkening or dimming, worsened vision or complete loss of vision. AAION generally involves symptoms from arteritis-related conditions that cause AAION. These symptoms can include:
In a small group of affected individuals, an “occult” form of arteritic ION is possible. That means they have vision loss but no other arteritis-type symptoms.
Arteritic and nonarteritic PION both cause sudden, painless vision loss. But PION is usually a progressive condition early on, meaning the symptoms get worse in the initial phase.
The causes for ION can vary depending on the type.
Experts aren’t sure exactly why NAION happens, but they think it’s usually due to several factors that add up and disrupt circulation in your optic nerve. The factors usually affect how your circulatory system regulates blood flow through your optic nerve. As long as that self-regulation works like it should, you won’t have NAION. But certain events or issues can disrupt that self-regulation. They include:
AAION and APION both have the same root cause: arteritis. This condition happens when there’s widespread circulatory system inflammation. The conditions most likely to cause this are:
Advertisement
NPION has only a few specific causes. They are:
Vascular risk factors increase the risk of ION. These include high blood pressure, diabetes, high cholesterol, smoking, sleep apnea and other factors listed above. And inflammatory diseases such as giant cell arteritis increase the risk of developing ION. ION happens more often among certain groups. For example, individuals over age 50, males and white people are more likely to develop ION.
An eye care specialist can diagnose ION using a combination of methods. The diagnosis process usually starts with asking you questions about your symptoms, recent life events, medical history and more. Your answers can help them narrow down the list of causes and rule out conditions similar to ION. They’ll also do an eye exam, with special emphasis on parts where they look at the optic disk at the back of your eye.
Advertisement
Several tests can help diagnose ION or a condition causing/contributing to it. Some of these are simple and minimally invasive or noninvasive. Examples of these include:
Some tests specifically diagnose or rule out arteritis-type conditions (which need specific treatments as soon as possible). These tests can include:
Advertisement
Your healthcare provider might recommend other tests depending on your symptoms and health history. They can tell you more about these tests and why you might need them.
The treatments for ION vary depending on the cause. Sometimes, a provider can treat ION directly. Other times, the only approach is to manage the vascular risk factors and focus on treating the symptoms.
Anterior and posterior arteritic ION need quick treatment with anti-inflammatory corticosteroid medications like prednisone or the immune-suppressing drug tocilizumab (Actemra®). Corticosteroids usually come in oral pill form but sometimes come in intravenous (IV) form (through a vein in your arm). The corticosteroid doses start high and gradually decrease over days or weeks. Some people may need to take low doses of these medications for an extended period to prevent ION from causing permanent vision problems.
Unfortunately, there’s no confirmed effective treatment for nonarteritic ION. Corticosteroid medications are usually not recommended when you don’t have an underlying arteritis-type condition.
For now, the main approach to treating nonarteritic ION is to manage the symptoms and treat or minimize any underlying causes and contributing factors. That’s important because nonarteritic ION usually affects one eye at a time, so this approach can lower your risk of having ION-related vision loss in both eyes.
If you have ION-related vision loss, your healthcare provider may recommend assistive devices like magnifiers or using magnification settings or voice commands/feedback on your devices. These can help you compensate or work around vision issues.
ION usually causes sudden vision loss. “Sudden” can mean it happens over minutes or hours, but sometimes. it can take days. The more common forms of ION cause blurring or weakened vision, while some forms cause total vision loss. Sometimes, people have brief episodes of blurred vision before they develop vision loss from ION.
ION isn’t life-threatening, but it can cause vision loss severe enough to disrupt your life.
ION may be reversible in some cases, but it usually causes at least some permanent vision loss. But people with vision loss also often learn to adapt to this condition and shift what areas of their vision they use for specific tasks like reading. When that happens, their vision may seem to improve, but it’s really that they’re better at working around their vision loss.
ION isn’t preventable, but you can lower your risk of developing it. The main way to do that is to prevent or manage conditions that can cause or contribute to ION. Your provider may recommend adjusting your blood pressure medication to avoid low blood pressure while sleeping, start you on medications to lower your cholesterol, adjust your diabetes medications, recommend quitting tobacco (including vaping) and other preventive measures to decrease your chances of developing ION.
ION is also something that medical professionals will take steps to prevent if you need to undergo surgery. If you have a history of ION or know you have a condition that could cause it (like GCA or vasculitis), tell your surgeon and/or anesthesiologist before your procedure so they can plan and adjust accordingly.
If you previously had nonarteritic ION in one eye, you’ll need to be vigilant for vision changes or loss in your other eye. That’s because having it in one eye makes you more likely to develop it in your other eye later on.
If you had arteritic ION, your eye care specialist will refer you to a specialist like a rheumatologist. A rheumatologist can help monitor and treat the underlying immune or inflammatory conditions causing your arteritis. It’s important to follow your eye care specialist and other providers’ guidance on managing your condition. That can help you prevent future flare-ups and additional vision loss or issues.
Your eye care specialist will schedule regular follow-up visits to monitor you for any changes in your vision or your eyes themselves. You should see them as recommended and contact them as soon as possible if you notice any changes in your vision. They can also tell you other specific changes that mean you need to call them or seek urgent medical attention.
Any sudden vision loss is an emergency symptom that needs immediate medical care. That’s because it can sometimes be a symptom of life-threatening conditions like a stroke or eye emergencies like a detached retina (which is reversible if treated quickly).
It takes a trained medical professional and specific tests to tell when sudden vision loss is truly an emergency issue, and minutes can make all the difference. That’s why you shouldn’t ignore sudden vision loss if you’ve never had it before. And if you have a condition that can cause or previously caused sudden vision loss, talk to your healthcare provider. They can explain when this symptom needs emergency care and when it’s something you should expect with your condition.
Some questions you may want to ask include:
No, but there are some similarities.
Ischemia is when cells stop working correctly and start dying because they aren’t getting enough blood flow. Ischemic strokes are when that happens in your brain. ION happens in your optic nerves, which is why they’re similar but not the same.
Another reason they’re similar is because people with ION can sometimes have early symptoms that go away. When that happens, it means you have a higher risk of developing optic nerve ischemia and vision loss in the following days. So, you shouldn’t ignore sudden vision loss, and having it means you should get emergency medical care right away.
The sudden vision loss that happens with ischemic optic neuropathy means your optic nerves aren’t getting enough blood flow. Over time, that can cause permanent damage and vision loss, so sudden vision loss is never something to ignore or wait on and see if it gets better.
If you have a condition that can cause sudden vision loss or ION, it’s a good idea to talk to your eye care specialist. They can tell you what to watch for and what to do if you notice vision changes. Acting quickly could make all the difference and help protect you from more serious vision disruptions and difficulties.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Getting an annual eye exam at Cleveland Clinic can help you catch vision problems early and keep your eyes healthy for years to come.
