Hypospadias is a congenital condition in which the meatus isn’t at the tip of the penis. Healthcare providers aren’t sure what causes it. Other symptoms include a curved penis and underdeveloped foreskin. It also may cause the pee stream to spray. A provider can diagnose it shortly after birth. Hypospadias usually requires surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
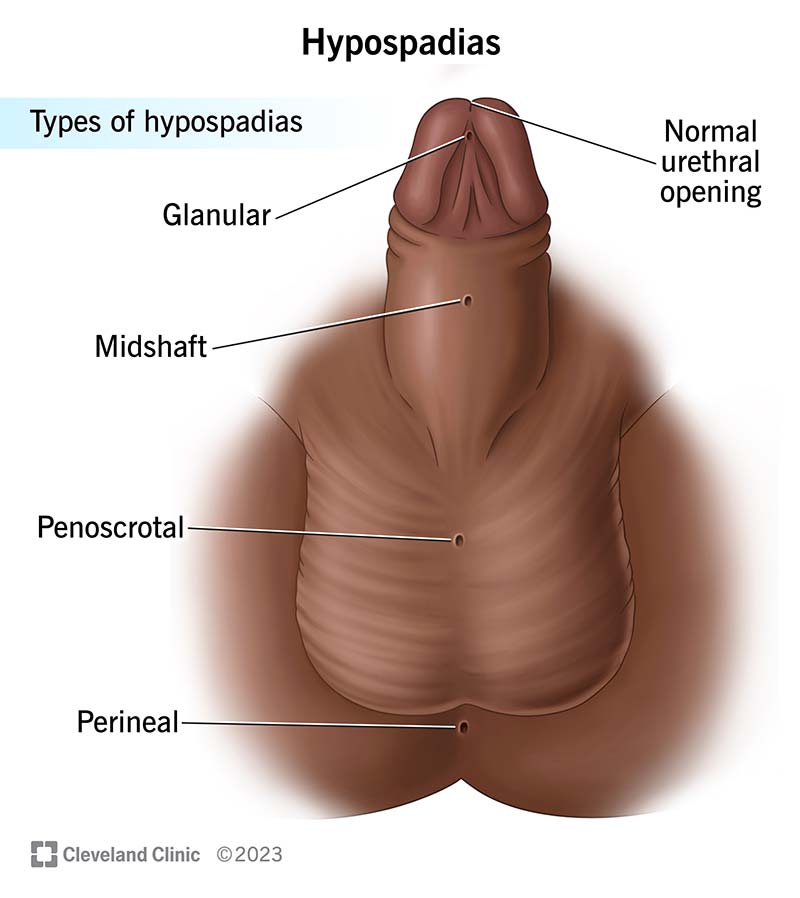
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/hypospadias)
Hypospadias is a condition where the urethra and foreskin don’t develop properly in a baby’s penis. The urethra is the tube that carries pee (urine) and semen (ejaculate) through the penis and outside of the body. The foreskin is the skin that normally covers the head of the penis completely in uncircumcised people.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Early in a fetus’s development, the urethra starts as an open channel. The channel closes to form a complete tube as a fetus develops before birth. The meatus is the opening at the end of the urethra. It’s usually in the head of or at the tip of the penis. It’s where semen and pee exit the body.
In a baby with hypospadias, the urethral tube doesn’t close all the way, causing the meatus to form below the tip of the penis. It may exist anywhere along the shaft of the penis, in the scrotum or even lower, near the butthole (anus). The scrotum is the pouch of skin behind the penis that usually holds the testicles. The anus is where poop exits the body.
Hypospadias is a congenital condition, which means it’s present at birth. It can range from mild to severe. Without treatment, problems can develop later in life, including difficulty peeing and difficulties having sexual intercourse.
Hypospadias can range from very mild to severe. A surgeon may not need to repair mild cases. But in most cases, hypospadias requires surgery.
Healthcare provides categorize the type of hypospadias by where the urethra opens:
Advertisement
Hypospadias is common. It occurs in approximately 1 of every 150 to 300 male infants. Only undescended testicles is more common. The milder forms happen more often than the severe forms.
The rate of hypospadias seems to be increasing in Western cultures. Researchers suspect there may be a link between rising rates of hypospadias and the increased use of certain chemicals, pollutants and pesticides.
The main symptom of hypospadias is that the meatus isn’t at the tip of the penis. Other hypospadias symptoms may include:
No, hypospadias and a chordee aren’t the same condition. But babies with hypospadias can sometimes have a chordee.
Healthcare providers and medical researchers don’t know exactly what causes hypospadias. Certain chemicals may increase the risk of hypospadias. There may also be a genetic link. A baby is more likely to have hypospadias if they have a biological relative who also had hypospadias.
Hypospadias can happen without any other medical problem. But providers often see it with other birth defects and congenital problems.
Hypospadias occurs during early pregnancy. The penis starts to develop around the eighth week of pregnancy. Hypospadias occurs between weeks nine and 12.
Certain factors may increase the risk of your baby having hypospadias. These include:
You may have difficulty getting pregnant with a partner through sexual intercourse if you have a more severe form of hypospadias or have a very bent penis due to hypospadias. Without treatment, hypospadias can create problems with the penis being able to enter the vagina and semen reaching the inside of the vagina. This can affect your ability to have biological children through sex and could result in male infertility.
Advertisement
You can pee with hypospadias, but it may be difficult to stand and pee. You may need to sit down so you don’t spray pee outside of the toilet.
Hypospadias is usually easy to diagnose because the meatus isn’t at the tip of the penis. Often, the foreskin doesn’t fully form or cover the underside of the penis as it normally should. Sometimes, the abnormal foreskin looks like a “hood” on the back of the penis. The penis may have a downward curve or bend. In more severe forms, the penis may be very small or short, and the scrotum may look like it’s separated into two halves.
Healthcare providers usually diagnose hypospadias shortly after birth. Checking for hypospadias is part of the routine newborn physical examination that a pediatrician performs. Sometimes, providers don’t catch hypospadias until they circumcise the baby. If your healthcare provider diagnoses hypospadias, they won’t continue the circumcision.
If a pediatrician detects hypospadias, they’ll refer you to a pediatric urologist. A pediatric urologist is a doctor who specializes in diagnosing and treating conditions that affect the urinary and reproductive systems in children.
Surgery (hypospadias repair) can treat hypospadias. Most pediatric urologists will perform a hypospadias repair when your child is between 6 and 12 months old. At that age, it’s easy to care for the surgery site after the procedure. It’s also safer for your child to have general anesthesia.
Advertisement
Surgery is usually an outpatient procedure (meaning your baby will go home the same day) and may take several hours to perform. Sometimes, healthcare providers must treat hypospadias in separate stages, especially if the hypospadias is more severe.
During hypospadias repair, the pediatric urologist will:
All types of surgery come with some risks, including:
Specific hypospadias repair risks include:
Advertisement
Recovery times may vary. Most children make a full recovery about six to eight weeks after a hypospadias repair. A healthcare provider will give you prescription medications to treat pain and prevent infection after surgery.
The outlook for hypospadias is good. Hypospadias repair has a high success rate. The goal of successful surgery is to create a penis that appears and functions normally.
If you're pregnant, you can reduce your baby's risk of having hypospadias by:
Before surgery, clean your baby’s penis normally during diaper changes and baths. There’s no need to forcefully pull back the foreskin or use any specific cleaning products.
After a hypospadias repair, follow your surgeon’s instructions. Keep your child’s affected areas as clean as possible to help prevent an infection. Wash your hands with soap and water before changing your child’s diaper or handling the area. If pee or poop gets on the area, gently clean the area with warm, soapy water and pat the area dry.
You should be able to sponge-bathe your child after a hypospadias repair. Carefully wash the area with soap and warm water. Pat the area dry with a towel. If your baby has a temporary catheter in place, ensure nothing pulls on it and that it drains appropriately. Once a provider removes the catheter, your baby can have regular baths again.
Your child should avoid lying on their stomach or playing on straddle toys, including a rocking horse, seesaw, swing, bicycle or jumper for two to three weeks.
Swelling, bruising and discoloration are very normal after hypospadias repair. They’ll gradually improve in one to two months.
Schedule follow-up appointments as recommended with your child’s healthcare provider. They’ll want to make sure your child’s penis is healing properly. If your child has a severe hypospadias, you may need to schedule more operations.
Take your child to the nearest emergency room if they experience any of the following symptoms after a hypospadias repair:
You may want to ask your child’s provider:
In most cases, there’s no association between hypospadias and any other conditions. But sometimes, there may be a link between hypospadias and intersex.
One study shows that children may inherit hypospadias equally between both biological parents.
Epispadias is also a congenital condition that affects the urethra. But the meatus forms at the top of the penis, not toward the bottom. Epispadias is a much rarer than hypospadias.
Hypospadias is a condition that affects babies at birth. The hole at the end of the urethra forms somewhere other than the tip of the penis. A healthcare provider can’t complete a circumcision during the newborn stage for most babies who have hypospadias. Hypospadias may lead to problems with peeing, sexual function and fertility later in life. It can be scary to hear that your baby might need surgical treatment. But hypospadias repair has a high success rate and good long-term results. Talk to a healthcare provider to learn more about this condition and treatment options.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When something’s wrong with your penis, you’ll want to get care right away. Cleveland Clinic’s experienced urology providers are here for you.
