A cervical polyp is a small growth on your cervix. It can cause vaginal bleeding. Your healthcare provider can detect polyps during a pelvic exam. Cervical polyps are usually removed and sent for testing. In most cases, cervical polyps are benign and not a cause for concern.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
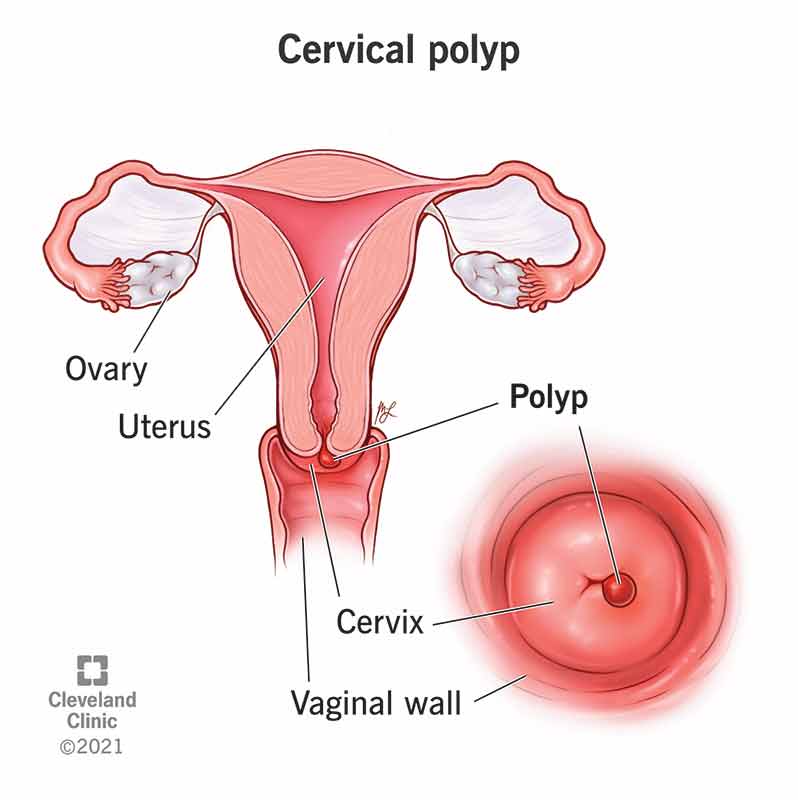
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24436-cervical-polyp)
Cervical polyps are small, irregular growths on the surface of your cervix or in your cervical canal. Your cervix connects your uterus to your vagina. A polyp on your cervix is rarely cancerous; however, some polyps can change into precancers. Your healthcare provider will recommend removing a cervical polyp if it’s causing symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Approximately 2% to 5% of women develop a cervical polyp. They’re most common shortly after your reproductive years and in people who’ve had more than one child. Cervical polyps are almost always benign (not cancer). Malignant (cancerous) polyps are more common in postmenopausal women but occur in less than 1% of all cases.
Most people never have symptoms of a cervical polyp. If you have symptoms, they could include:
Most polyps are elongated, tear-shaped growths that stick out from your cervix. They’re smooth or slightly spongy in texture and bright red, pinkish to purple or greyish-white. Some polyps have a long, thin stalk (called a pedicle) attached to them. They’re usually less than a half-inch long but can grow larger. They can bleed when you touch them.
Cervical polyps are caused by:
Advertisement
A cervical polyp is usually diagnosed during a pelvic exam or Pap test. Your healthcare provider will be able to see a polyp once they insert a speculum into your vagina. A speculum is a device that opens the walls of your vagina to better see your cervix.
Healthcare providers typically diagnose a polyp during a speculum exam. Further tests aren’t usually necessary to diagnose a cervical polyp. Your provider removes the polyp, then sends it to a lab for analysis.
In some cases, your healthcare provider will order an ultrasound to evaluate the area around the cervical polyp. A biopsy of the cervical tissue determines if the polyp is malignant. It’s rare for a cervical polyp to be malignant (cancerous).
Yes, removing a polyp is the safest approach most of the time. Your provider will remove any polyps that cause bleeding or other symptoms during a pelvic exam (usually right after diagnosis). If the polyp is large, your healthcare provider may want to remove it in a surgical center in case there are complications.
They’ll send the polyp to a lab for testing to ensure there are no signs of cancer.
The removal of a polyp is called a polypectomy. This typically happens in your provider’s office during a pelvic exam. Your healthcare provider may perform the surgery in a surgical center or operating room with anesthesia (if the polyp is large).
Your provider removes small cervical polyps by pulling or twisting them off with a pair of forceps. You aren’t under anesthesia, and it’s a relatively quick and painless procedure. If there isn’t a base or stalk to grasp or the polyp is large, your healthcare provider may use loop electrosurgical excision procedure (LEEP). This is a surgical method that uses a wire loop heated by an electric current to burn the polyp from the surface of your cervix. Your provider numbs your cervix with an anesthetic before LEEP.
Complications are rare. Having a cervical polyp removed could cause:
You can expect to feel mild cramping after polyp removal. Most people will have light bleeding afterward. Using an over-the-counter (OTC) pain reliever like acetaminophen or ibuprofen can help. You shouldn’t have sex or wear tampons for at least two weeks or until the bleeding has subsided. Talk to your healthcare provider about what to expect after the procedure.
The most common side effects are light bleeding and cramping. This should subside within a few days. Getting a polyp removed is a quick, safe procedure that rarely causes any complications. You should be able to resume your usual activities within a day or two after getting a polyp removed.
Advertisement
Most cervical polyps are benign and easy to remove. Your healthcare provider will recommend removing the polyp if they feel it’s necessary. There are no long-term complications of having a cervical polyp.
It’s rare for cervical polyps to grow back, but it can happen. You may be more likely to develop cervical polyps if you’ve had them in the past.
Cervical polyps are uncommon during pregnancy. They’re usually small and don’t cause symptoms. Some healthcare providers will recommend removing a cervical polyp during pregnancy, but others will advise against it because it could disrupt your cervix. If you develop a polyp while pregnant, your provider may or may not remove the polyp. It depends on your condition, the size of the polyp and its location.
Cervical polyps are hard to prevent, but you can take certain steps to reduce your risk of infection like practicing safe sex (using a condom). Other causes of cervical polyps are out of your control. Getting regular pelvic exams and Pap tests is the best way to find and treat polyps before symptoms start.
Call your healthcare provider if you have any of the following symptoms:
Advertisement
Having regular pelvic exams is the best way to detect cervical polyps. Always let your healthcare provider know if you experience irregular vaginal bleeding. If you’re diagnosed with a polyp on your cervix, it’s usually not a cause for worry because most don’t cause problems or lead to cancer.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From routine pelvic exams to high-risk pregnancies, Cleveland Clinic’s Ob/Gyns are here for you at any point in life.
