A spermatocele is a common growth that develops above or behind your testicle. They’re benign (not cancer). You may not have any symptoms or notice a spermatocele. Healthcare providers usually only treat it when a large spermatocele hurts or bothers you.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
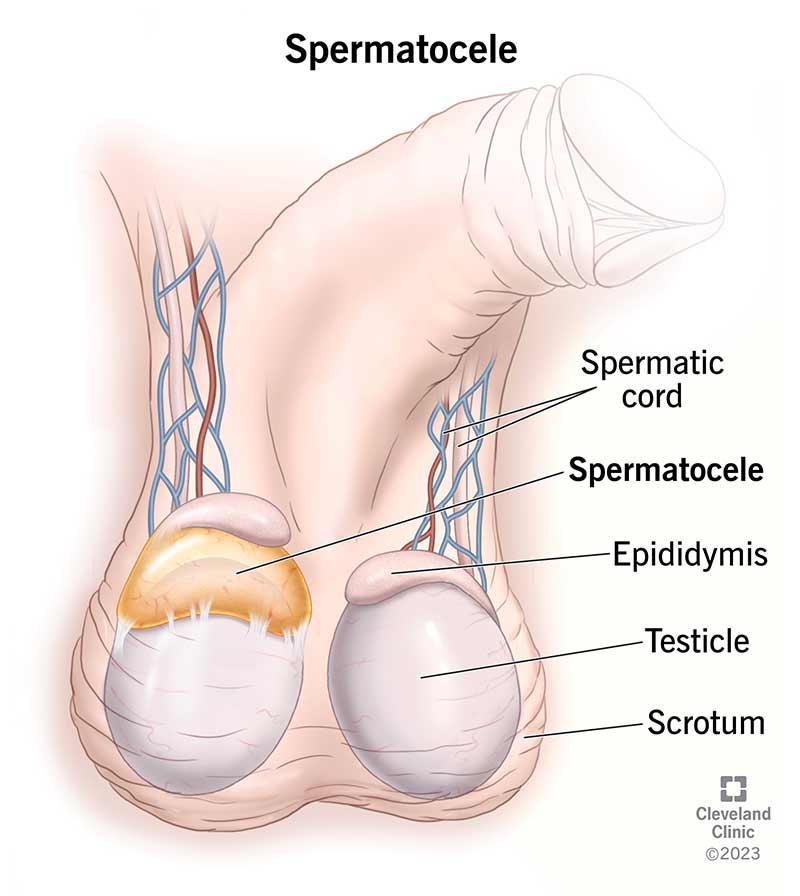
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17492-spermatocele)
A spermatocele is a fluid-filled growth (cyst) that develops from your epididymis. Your epididymis is a tube that runs behind and over the top of each testicle. Its main job is to store and transport sperm. Sperm are male reproductive cells.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Spermatoceles can develop above or behind your testicles (testes). Inside each spermatocele is a clear or cloudy fluid that may contain sperm.
Other names for spermatoceles include spermatic cysts or epididymal cysts.
Spermatoceles don’t typically hurt, so you may not notice a lump right away. Even if there isn’t pain, it can be scary to notice a lump around your testicle. Talk to a healthcare provider if you notice changes to your testicles. Talking to a healthcare provider about any changes to your testicles is the first step in getting an official spermatocele diagnosis and soothing any frightening thoughts or feelings.
Spermatoceles are fairly common. They affect nearly 1 in 3 adult males.
Smaller spermatoceles usually cause few or no symptoms. They may not bother you at all. Depending on the size, larger spermatoceles may cause mild to moderate symptoms, including:
Spermatoceles vary in size. They may look like:
Advertisement
Spermatoceles feel like a smooth, hard lump.
Spermatoceles occur when sperm builds up somewhere in the epididymis. Healthcare providers don’t fully understand what causes sperm to build up. Some experts believe that a blockage in the epididymal duct or inflammation may be potential causes.
In many cases, spermatoceles appear without any sign of injury, bacterial infection or other obvious cause.
No, a spermatocele isn’t a sexually transmitted infection (STI), and it isn’t contagious. If you have a spermatocele, you can’t give it to another person.
Spermatoceles can affect anyone with testicles at any age. But they most commonly appear in midlife (40s or 50s).
No, ejaculating won’t make a spermatocele increase in size.
Spermatoceles usually don’t cause any symptoms. A healthcare provider typically detects a spermatocele during a routine physical examination or medical test for another issue. Some people discover a spermatocele while performing a testicular self-exam.
A healthcare provider may perform or order tests during or after a physical exam. These tests can reveal more about a testicular lump or rule out other testicular disorders:
Spermatoceles won’t likely go away without treatment.
Most spermatoceles remain small in size and cause few or no symptoms. You don’t need treatment if a spermatocele doesn’t cause pain or discomfort.
If you have long-term pain or discomfort, a provider may recommend surgery to get rid of a spermatocele.
A healthcare provider who specializes in conditions that affect your urinary system and reproductive system (urologist) performs surgery to remove a spermatocele (spermatocelectomy). Sometimes, the procedure may require your urologist to remove part or all of the epididymis (epididymectomy).
A spermatocelectomy is an outpatient procedure. That means you can go home after surgery instead of staying in the hospital for a day or more.
During a spermatocelectomy, your surgeon makes a cut (incision) in your scrotum or groin area. They’ll access and remove the spermatocele from this incision.
An anesthesiologist may use local or general anesthesia. Local anesthesia numbs the general area and keeps you comfortable as you lie awake for the procedure. If you receive general anesthesia, you won’t be awake or feel any pain during the procedure.
In general, a spermatocelectomy is a safe, routine procedure that should improve your spermatocele symptoms.
Advertisement
Spermatoceles usually don’t go away on their own without treatment.
Spermatoceles are a pretty common condition. They usually cause few or no symptoms. They usually don’t cause further health issues or pose a serious threat. Many times, people don’t know they have a spermatocele because they don’t realize it’s there, so healthcare providers don’t check for them.
Larger spermatoceles may be painful or uncomfortable. In these cases, a spermatocelectomy may provide relief.
No. Spermatoceles are benign (noncancerous) cysts, which means they aren’t cancerous. There isn’t any evidence to suggest spermatoceles can turn into cancer. And having a spermatocele doesn’t increase your risk of developing testicular cancer.
No, spermatoceles don’t cause male infertility. However, surgery can cause blockage of your epididymis, which could affect your fertility. If you’re concerned, talk to a healthcare provider. They can explain your treatment options, including how therapies may affect your ability to have biological children.
Your affected areas need time to heal after a spermatocelectomy. It’s a good idea to take at least three to four days off from work or school. You may need to take more time off if you have a physically demanding job.
Advertisement
No, you can’t do anything to lower your risk of developing a spermatocele. But for many people who have spermatoceles, the cysts don’t cause any problematic symptoms.
Call a healthcare provider if you:
Go to the nearest emergency room if you have worsening testicular pain and swelling that comes on suddenly with no apparent cause.
A hydrocele is benign fluid that fills the sac in which the testicle sits in your scrotum. In most cases, hydroceles aren’t serious or painful. It’s possible for them to remain stable for many years. But sometimes, they’re large and require treatment.
Spermatoceles are common, usually painless testicular cysts that tend to affect people in midlife. But noticing a lump near your testicle can be unnerving. It’s a good idea to reach out to a provider. They can perform an evaluation and provide answers and set your mind at ease. You likely won’t need treatment if a spermatocele doesn’t bother you.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
If you have a condition that’s affecting your urinary system, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
