The genitourinary syndrome of menopause (vaginal atrophy or atrophic vaginitis) frequently affects women transitioning to menopause. It’s a condition where the lining of your vagina gets drier and thinner from a lack of estrogen. Burning, itching, spotting and pain with sex are common symptoms, as are frequent urination and urinary tract infections.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
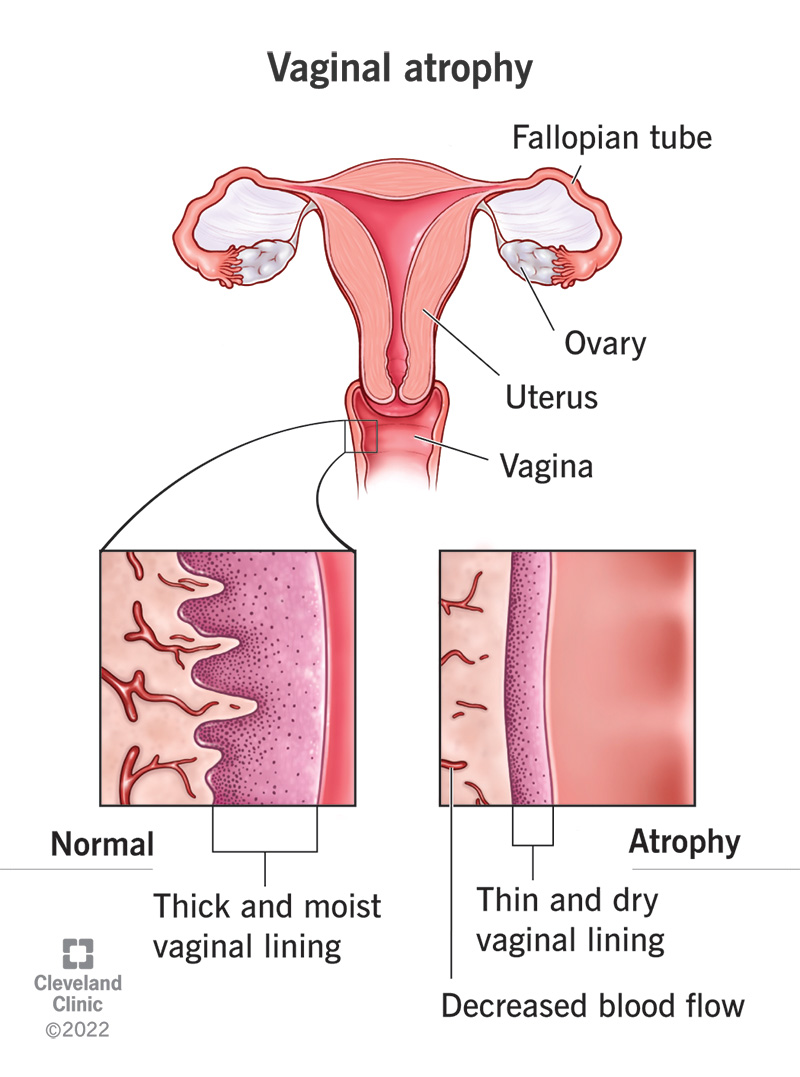
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15500-vaginal-atrophy)
Vaginal atrophy is a condition where the lining of your vagina gets drier and thinner. This results in itching, burning and pain during sex, among other symptoms. The condition also includes urinary tract problems such as urinary tract infections (UTIs) and urinary incontinence.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Vaginal atrophy most often occurs during perimenopause and menopause when your ovaries produce less estrogen. It can occur when your estrogen levels decrease due to cancer treatment or having your ovaries removed. You may experience many uncomfortable symptoms when hormone levels decrease. These symptoms can disrupt your quality of life.
Recently, the term vaginal atrophy has been replaced with the newer term, genitourinary syndrome of menopause (GSM). This new term helps describe not just the vaginal, but also the urinary symptoms that may occur as a result of low estrogen.
At least half of women who enter menopause show signs and symptoms of genitourinary syndrome of menopause. Vaginal dryness is typically the first indication that you're developing vaginal atrophy.
The tissue that lines the wall of your vagina becomes thin, dry and inflamed when you have vaginal atrophy. Often, the first sign is less lubrication (dryness), which you may notice during sex. Other symptoms of genitourinary syndrome of menopause include:
Advertisement
It can also affect your urinary system and cause symptoms like:
During menopause, your body makes less estrogen. Without estrogen, the lining of your vagina can become thinner and less stretchy. Your vaginal canal can also narrow and shorten. Less estrogen also lowers the amount of normal vaginal fluids and changes the acid balance in your vagina. All of these factors make your vaginal tissue more delicate and more likely to become irritated.
Your body can also produce less estrogen during events other than menopause. If you're breastfeeding, receiving treatment for cancer or have had your ovaries removed, you can experience vaginal atrophy due to lack of estrogen.
Women in menopause are the most likely to experience vaginal atrophy because their body naturally produces less estrogen. However, other factors can decrease estrogen levels and lead to vaginal atrophy. These include:
If you have penetrative sexual activity less often (with or without a partner), you may also have a higher risk of moderate to severe vaginal atrophy. Studies show that people who have sex more often tend to have milder cases of atrophy than those who stop having sex. This is because sexual stimulation increases blood flow to your vagina and makes your vaginal tissue more elastic.
Vaginal atrophy can affect your quality of life and your relationship with your partner(s). There are physical and emotional side effects of GSM. Physical symptoms like pain, burning, itching and leaking pee can disrupt all areas of your life. Emotional side effects are just as complicated as the physical side effects. If you're experiencing symptoms of vaginal atrophy, you may lose interest in sex and intimacy or lose confidence in yourself. Please know that all of these feelings are normal and that your healthcare provider is there to help you.
A healthcare provider can diagnose vaginal atrophy based on your symptoms and a pelvic exam to look at your vagina and cervix. Classic signs of atrophy during a pelvic exam include:
Advertisement
While healthcare providers typically rely on examinations to diagnose atrophic changes or GSM, they may do the following tests to rule out other conditions:
It's common to feel uncomfortable discussing symptoms of vaginal atrophy. Don’t feel ashamed to mention it to your healthcare provider if you think you have symptoms. There are several different treatment options available and most are successful in treating your symptoms.
Estrogen therapy and dehydroepiandrosterone (DHEA) are the only hormone therapies for vaginal atrophy.
Topical vaginal estrogen treats symptoms of vaginal atrophy without increasing levels of estrogen levels in your bloodstream. It’s available in a cream, a vaginal pill or a ring. Your healthcare provider can discuss each option with you and which may work best for you.
Advertisement
Also called systemic estrogen therapy, this type of hormone therapy may be helpful if you have other symptoms of menopause such as severe hot flashes. This is taken in higher doses that go to other cells of your body, not just to your vagina. If you’re more than 10 years past menopause or only have vaginal dryness, you’ll probably use local therapy. If you do need systemic hormone therapy, there are benefits, such as improved vaginal health, better sleep, fewer hot flashes and improved mood. You and your healthcare provider can discuss if systemic hormone therapy is right for you.
You and your healthcare provider will work closely together to come up with a treatment plan for vaginal atrophy. They’ll help you decide which plan is most effective based on your symptoms and the severity of them. Estrogen and DHEA therapy are considered to be the most effective. However, these therapies aren’t for everyone. There are several treatment options available that don’t involve hormones.
Lubricants and moisturizers treat vaginal dryness. This improves comfort during sex. Multiple brand names are available over the counter at your local grocery store.
Vaginal lubricants should be used during intercourse to reduce friction and pain with sex. They’re water, silicone or oil based. These products are very short-acting.
Advertisement
Vaginal moisturizers adhere to the vaginal tissue to help the cells maintain moisture. They’re applied every one to three days as they’re longer acting.
Some natural oils, such as olive and coconut oil, may also be used as lubricants and moisturizers.
Noninvasive and nonsurgical CO2 laser treatments help regenerate vaginal tissue and improve its strength and elasticity after laser treatments. These devices aren’t yet approved by the Food and Drug Administration for vaginal atrophy because there’s limited long-term research on their use.
Dilators are devices to widen (dilate) your vagina to improve comfort during sexual intercourse. People often start with a small dilator and slowly advance to larger sizes over time.
Osphena is a pill you take each day. Its benefits are similar to those of estrogen, but it doesn’t contain estrogen. A serious but uncommon side effect is increased risk of blood clots. You may notice more hot flashes, though most people have no symptoms.
Pay attention to any new symptoms that come after you start treatment. These could include skin irritation, more pain and/or vaginal discharge. Discuss any possible side effects with your healthcare provider. Don’t hesitate to consult them if you’re uncomfortable with your treatment plan.
The time it takes to treat symptoms of GSM vary depending on what method you use and the severity of the condition. Your healthcare provider can discuss all possible options with you based on your health history and your situation. They’ll work with you to determine the most successful treatment plan. Keep in mind that many people find success combining treatments.
You don’t have to just “live with” vaginal atrophy. Even if you’re in menopause or postmenopausal, that doesn’t mean you should have to deal with UTIs, vaginal itching or painful sex. Treatment for GSM can be very successful. Don’t be afraid to try different treatments and work with your provider on a method that works best for you.
Vaginal atrophy can’t be cured, but you don’t have to live with the discomfort. With proper diagnosis and treatment, the symptoms can be managed.
Yes, it can. That’s why prompt treatment is important. The sooner you get treatment, the less likely it is that your vaginal atrophy will worsen. For example, the longer you go without estrogen, the dryer your vagina will become. Without treatment, your vaginal atrophy may get worse. Occasionally, atrophy can become so severe that it can significantly narrow your vaginal opening. This may make it harder to treat the atrophy if treatment is started too late.
Losing estrogen is part of your body’s natural aging process.
However, there are ways to keep vaginal atrophy from getting worse. Avoid vaginal irritants such as perfumes, dye, shampoo, detergents and douching.
Remember, regular sexual activity is good for vaginal atrophy because it increases blood flow to your vaginal tissue.
Vaginal atrophy can seriously affect your quality of life in general, not just your sex life. The pain, dryness, burning/itching, spotting, bleeding, urinary problems, UTIs and discharge can make you very uncomfortable and interfere with your daily living. One in 4 women report that vaginal atrophy has had a negative impact on other areas of their lives including their sleep, sexual health and general happiness.
Prioritize your sexual health as much as any other aspect of your health. Look to your healthcare provider for answers to any questions and concerns.
Even if you’re not in menopause, be sure to report any symptoms of dryness, pain, burning/itching, urinary problems, unusual spotting or bleeding or discharge to your healthcare provider.
If weeks go by and the over-the-counter moisturizers you’re using for dryness don’t work, you should see your healthcare provider.
Also, always see your healthcare provider for any symptoms that negatively impact your daily life.
Both vaginal atrophy and yeast infections can have symptoms of dryness, itching, redness and pain. However, lack of estrogen causes vaginal atrophy while a fungal infection causes a vaginal yeast infection. Consult with your healthcare provider regarding symptoms so that, together, you can determine what condition you have.
Vaginal atrophy is serious. It affects your quality of life with discomfort, frequent bathroom trips, frequent UTIs, burning, pain with sex and more. Fortunately, there are many treatments and your healthcare provider can help you find the best option for your symptoms.
Seek treatment. Don’t be afraid to have the conversation with your healthcare provider and with your partner(s). Always follow your healthcare provider’s instructions and do what you can to manage vaginal atrophy.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Menopause is natural, but it also can disrupt your life. Cleveland Clinic is here to help you get relief.
