Patent ductus arteriosus (PDA) is a heart condition that affects some babies (more often, those born prematurely). PDA causes problems with blood flow between the heart and lungs. PDA sometimes resolves on its own. When it doesn’t, healthcare providers treat PDA and restore normal circulation with medication, catheterization and surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
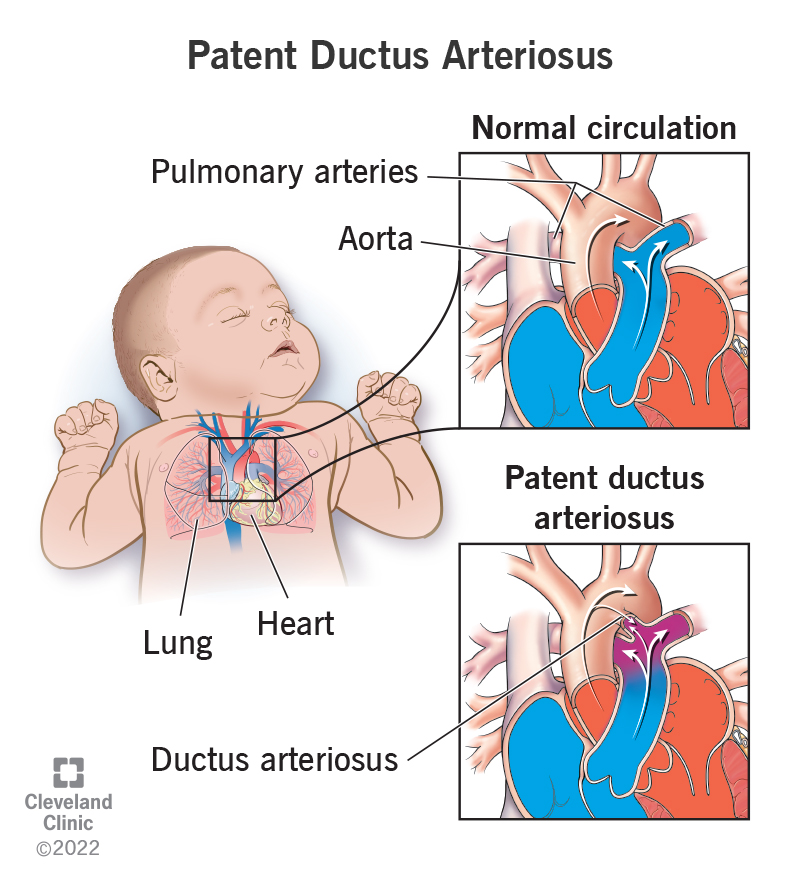
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17325-patent-ductus-arteriosus)
Patent ductus arteriosus (PDA) is a heart condition in babies. It happens when a blood vessel called the ductus arteriosus doesn’t close as it should after birth.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
During fetal development (before a baby is born), very little blood flows to a baby’s lungs. Instead, most of the blood bypasses the baby’s lungs. One way for this to happen is that blood flows from the main heart artery (aorta) to the primary lung artery (pulmonary arteries) through a special fetal blood vessel (ductus arteriosus). This blood vessel usually closes during the baby’s first few days of life when the blood flows to the baby’s lungs.
When a baby has a PDA, the ductus arteriosus doesn’t close properly. A small opening is left. The opening allows extra blood from the aorta to enter the baby’s lung arteries. Depending on the size of this blood vessel, your baby’s heart and lungs may have to work harder to pump blood.
Babies born prematurely are more likely to have a PDA. The condition is also more common in girls than boys.
Patent ductus arteriosus is the most common heart condition in newborns. Healthcare providers diagnose the condition more often in premature babies. The risk increases the earlier the baby is born. PDA happens in about:
Advertisement
A moderate or large PDA can cause babies to breathe faster and harder than normal, as their bodies try to keep up with the extra blood in their lung arteries. If left untreated for a prolonged period, a PDA can lead to the development of pulmonary hypertension (high blood pressure in the lungs) and blood vessel damage.
Researchers don’t know for sure why this condition happens. Patent ductus arteriosus causes may include genetic disorders or a family history of the condition. Other PDA causes may include:
PDA symptoms vary according to patent ductus arteriosus types. Small PDAs may not cause any symptoms other than a heart murmur.
Larger PDAs may cause:
If you notice symptoms of a PDA in your baby, tell your healthcare provider. Your provider may hear a patent ductus arteriosus heart murmur during a well-baby care visit or physical examination.
If your healthcare provider suspects PDA, they may recommend referral to a specialist, a pediatric cardiologist. The pediatric cardiologist may order certain tests, including:
Healthcare providers sometimes diagnose PDA in adults. If you had a small PDA as a baby, you may not have gotten treatment. Symptoms can include:
Your healthcare provider will consider your baby’s age, size and health when determining a treatment plan. They might recommend observation (watchful waiting) to see if the PDA will close on its own. A watchful waiting approach involves regular checkups and tests so the provider can see if the PDA is closing. Occasionally, treatment may not be necessary.
Healthcare providers may treat patent ductus arteriosus with medication, including nonsteroidal anti-inflammatory drugs (NSAIDs). Medications may encourage patent ductus arteriosus closure. This is commonly used in premature babies, but not in older children or adults.
Advertisement
Healthcare providers may treat PDA with surgical procedures, including:
After catheterization or surgery, blood flow returns to normal immediately if there are no other heart defects.
Closing the PDA gets blood flow back to normal. After closure via a cardiac catheterization, your child will take antibiotics for six months to prevent heart infection (endocarditis). Your healthcare provider will discuss the necessary follow-up care with you.
Adults who have PDA closure procedures will also take antibiotics for six months and should see a cardiologist for follow-up care.
With treatment, most babies born with PDA live healthy and active lives.
Advertisement
If PDA doesn’t close on its own, healthcare providers can correct it, if needed. Babies and children with moderate and large sized PDA’s that are not treated in the correct timeframe may be at higher risk for developing heart complications as adults. Talk with your healthcare provider about whether your baby needs follow-up care.
There isn’t anything you can do to prevent PDA.
If you have rubella during pregnancy, your baby may be at higher risk of developing PDA. Tell your healthcare provider right away if you’re exposed to rubella during pregnancy.
Follow all instructions from your healthcare provider. Keep all follow-up appointments and let your provider know right away if your baby develops new symptoms.
Call your provider if your baby develops new symptoms. If your baby has trouble breathing, seek emergency care right away.
Patent ductus arteriosus (PDA) is a congenital heart condition. With treatment, your child can live an active and healthy life. Talk with your healthcare provider about the best treatment options.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Learning your baby has patent ductus arteriosus can be stressful. Cleveland Clinic Children’s experts craft a personalized treatment plan to match your child’s needs.
