You’ll feel some pain after having any type of surgery. It’s part of your body’s healing process. No option is automatically the best for everyone, but your surgeon will suggest a combination of medications to help you feel comfortable while you recover.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
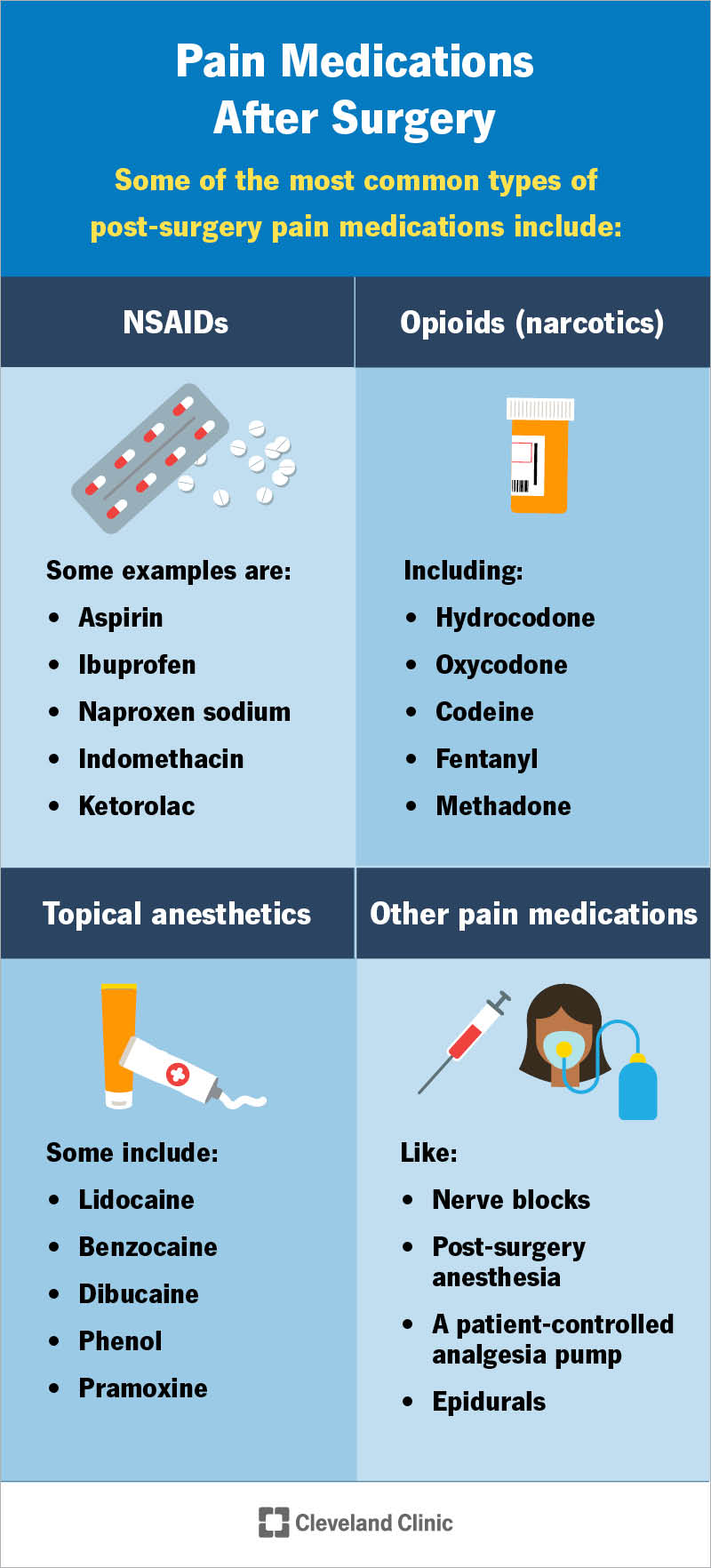
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/pain-medication-after-surgery)
Everyone feels some pain after surgery. It doesn’t matter whether you’re having a planned operation or emergency trauma surgery. You’ll feel pain from the surgery itself and as your body heals. Managing that pain is an important part of the healing process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you know you’re going to need surgery, talk to your surgeon about pain management ahead of time. They’ll answer any questions you have and help you know what to expect. You may want to talk to your surgeon about:
Your surgeon will suggest a combination of pain management techniques to help keep you comfortable and safe after surgery. For most people, that includes at least one kind of medication.
How your body responds to a surgery will depend on lots of factors. The type of surgery you have, your natural pain tolerance and age can all affect how you feel after an operation. You’re probably expecting to feel pain around your surgery site, but you might also feel:
Advertisement
Pain can cause a variety of different feelings. The pain may feel:
Tell your care team where it hurts and how the pain feels. This will help them understand what’s going on inside your body so they can manage the pain.
There’s no single medication that’s best for everyone. Your body, health and post-surgery healing process are unique. Something that’s a good option for you may not work for someone else.
There are several kinds of pain medications your surgeon may give you after surgery. They may give you IV (intravenous) infusions of medications if you’re staying in the hospital. Many of the most common pain medications you’ll need are pills that you’ll take by mouth (orally).
Some of the most common types of post-surgery pain meds include:
NSAIDs relieve pain and reduce inflammation. Your surgeon may suggest over-the-counter NSAIDs or a prescription-strength version. Common NSAIDs include:
Opioids are prescription medications that bind to receptors in your brain and body to reduce pain signals. Opioids are powerful medications and can be addictive. Many healthcare providers are prescribing opioids less often or in smaller doses to reduce the risks of complications. There are more than 100 types of opioids, including:
Topical anesthetics are medications that numb a specific part or area of your body. Providers sometimes call them local anesthetics. Your surgeon may prescribe a topical anesthetic that keeps the area around your surgery site numb. These can include patches, creams or ointments that you put on your skin. Common local anesthetics include:
Your surgeon may suggest other medications alongside some of the types above. For example, you might need over-the-counter or prescription acetaminophen (Tylenol®) or a muscle relaxer.
If you’re staying in the hospital after a major surgery, your care team may use specific pain medications like:
It might seem obvious, but reducing how much pain you feel is the biggest benefit of taking pain medication after a surgery. This isn’t just about keeping you comfortable. Although that’s an important part of pain management. Your body heals faster when you’re not in pain. Reducing your pain can actually help speed up your recovery.
Managing pain can also reduce the risk of complications after a surgery. If the pain is well-managed, it will be easier for you to walk, move or breathe deeply. This can reduce your risk of pneumonia, blood clots and other issues.
Advertisement
All medications can cause side effects. Some of the most common side effects of pain medications can include:
Opioids can be habit-forming and cause opioid use disorder. If you take too many at once (or too often), you can experience an opioid overdose, which can be fatal. Your surgeon will check your medical history and addiction risk before giving you opioids. Tell them if you or anyone in your biological family has a history of substance use disorders.
Your care team will discuss the risks of side effects and complications of any medications you’ll need. Tell them if you’re worried about any specific risks or if you’re unsure about how you’ll respond to medications. They’ll help you find safe, effective options to manage the pain.
How quickly a pain medication starts working can vary. Most medications should start reducing the pain within an hour or two. Ask your care team how quickly you should feel your medicine working. They’ll let you know what to expect.
Your surgeon will give you specific instructions about taking pain medicine. They’ll tell you how much medicine you can take and how often it’s safe for you to take it.
Advertisement
You may not feel enough pain to need medicine as often as you’re allowed to take it. That’s OK. If you aren’t feeling pain, it’s usually safe to skip a dose and wait until the pain gets worse or it’s the next scheduled time to take your medication. Ask your surgeon if it’s safe for you to skip doses if you’re not in pain.
Your surgeon may also suggest that you take your medications on a set schedule, whether or not you feel intense pain. This can help you “stay ahead” of pain to avoid feeling a lot all of a sudden.
Ask your surgeon which pain management plan they think is best based on the surgery you had and the medications you’re taking.
Talk to your surgeon if you feel like you’re in more pain than you should be. They might be able to adjust your dose. Post-surgery pain meds can have complex interactions with medications you have at home.
Your surgeon can also adjust which type of medication for pain you’re using. Some medications (especially opioids) have a limited dose and you may not be able to get more after you’ve finished the initial course.
Don’t feel guilty about calling or talking to your care team if you’re hurting. Some people feel like they’re “bugging” their care team with questions. It’s always OK to ask your doctor these questions. Your providers are there to help, no matter what. Making sure you’re healing properly is always important to them.
Advertisement
Never take more medication than your care team says is safe. You’re much more likely to experience severe complications if you take too much pain medicine.
Most of your pain management will happen at home after you leave the hospital or surgery center. Taking your medications will be part of your pain management plan, but you may also want to:
Your surgeon will tell you how often you’ll need follow-up visits. They’ll make sure you’re healing properly and that your recovery is going smoothly.
Call your surgeon or care team if you notice any signs of complications, including:
Having surgery hurts. But even though you’ll experience some pain after an operation, that doesn’t mean you need to be in agony while you recover. Your surgeon will suggest pain medications to help you feel comfortable. They’ll tell you how to take them, how much is safe to take and when it’s OK to take more. All medications can have side effects, but your surgeon will help you understand all the risks ahead of time.
Ask your care team any questions you think of before and after your surgery. They’ll explain everything you need to know. It might help to have a loved one take notes if they’ll be with you. You can always ask your care team for a printout of instructions and guidelines so you can reference them later.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Sometimes you have surgery planned. Other times, it’s an emergency. No matter how you end up in the OR, Cleveland Clinic’s general surgery team is here for you.
