The ideal fetal position for labor is when the fetus is head down, facing your back, with its chin tucked to its chest and the back of the head ready to enter your pelvis. This is called cephalic or occiput anterior presentation. Most fetuses settle into this position by the 36th week of pregnancy. Other fetal positions, like breech presentation, make a vaginal delivery more challenging.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
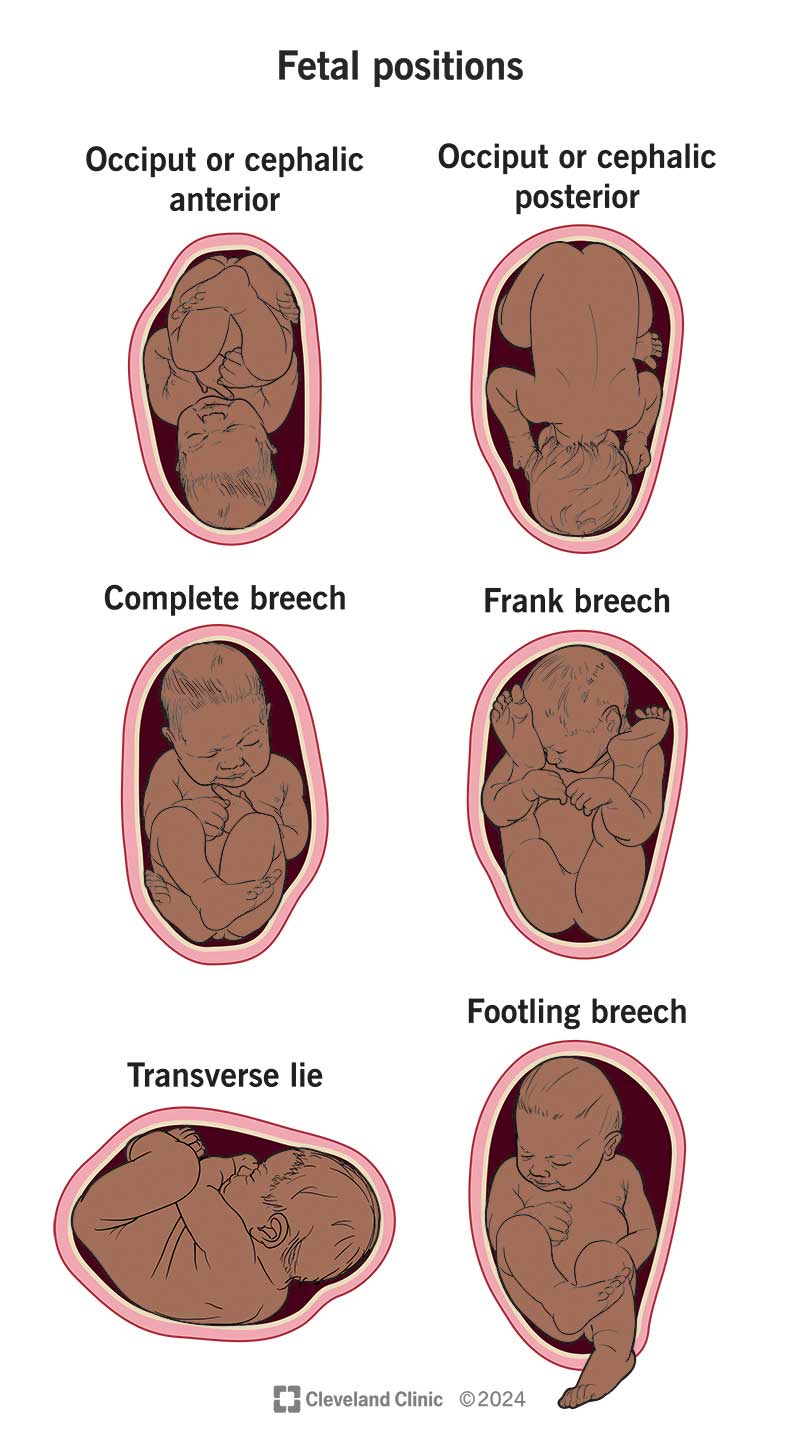
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9677-fetal-positions-for-birth)
Fetal positioning refers to a fetus’s position in your uterus before birth. Your pregnancy care provider may call it fetal presentation or the presentation of the fetus (although this usually refers to which part of a fetus’s body will move into the birth canal first). Knowing the position of the fetus helps a pregnancy care provider determine if it’s safe for you to have a vaginal delivery or if they should consider a C-section (cesarean delivery).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
During childbirth, your healthcare provider’s goals are to safely deliver your baby and make sure you’re healthy after delivery. A vaginal delivery can become more challenging, or even unsafe, if the fetus is in certain positions.
Sometimes, your baby doesn’t get into the perfect position before birth. There are several positions that a fetus can be in, and some of these positions could come with complications during childbirth.
Possible fetal positions can include:
Advertisement
All breech positions increase your chances of having a C-section delivery because a vaginal delivery can become unsafe. In many cases, your healthcare provider will recommend a C-section instead of a vaginal birth.
Ideally, the fetus is head down, facing the birth mother's back, with its chin tucked to its chest. This position is called cephalic or occiput anterior presentation. It’s the safest fetal position because it carries the least amount of risk to both the birth mother and the fetus. It’s very common for a fetus to turn into this position naturally by the 36th week of pregnancy.
Fetal attitude describes the position of specific parts of a fetus’s body. The ideal fetal attitude is when the fetus has its:
But, there can be times the fetal attitude is irregular. For example, its chin is tilted back instead of tucked.
Fetal lie describes how the fetus’s spine lines up with its birth mother's spine. Ideally, they line up vertically because the fetus’s head is down in the birth canal. This is called longitudinal lie. If the fetus is sideways or horizontally across the uterus, it’s in a transverse lie.
Your healthcare provider will check fetal positioning by touching or gently pressing on parts of your abdomen during your regular prenatal appointments. This will happen during most of your appointments in the third trimester. If your provider is unsure, they may also do an ultrasound to check fetal positioning.
Breech position is probably the most unfavorable fetal position because it comes with the most risks. There are several different types of breech positions, and each position comes with its own potential dangers. Your pregnancy care provider can discuss these risks with you and let you know what they feel is the best way to deliver your baby.
Before delivery, there’s no risk to a fetus in a breech position. But there are risks to attempting a vaginal delivery on a fetus in the breech position.
Typically, the fetus moves into position for birth in the third trimester. This happens in the last few weeks of your pregnancy (often between weeks 32 and 36).
There are several ways that your healthcare provider can try and turn the fetus before you go into labor. These methods don’t always work, but if they can be done safely, your provider may recommend giving it a try.
The most common way for a provider to turn a fetus is external cephalic version (ECV). But there are other techniques you can try at home on your own. Even though there isn’t a guaranteed success rate, these at-home methods are usually worth a try.
ECV is one noninvasive way to turn the fetus and improve your chances of having a vaginal birth. Your pregnancy care provider performs ECV in the labor and delivery unit in case of a complication. This procedure involves a provider lifting the fetus’s buttocks in an upward position and then applying pressure through the abdominal wall to your uterus to rotate the fetal head forward or backward. The best time to perform this procedure is between 36 to 38 weeks of pregnancy.
Advertisement
Sometimes, you can encourage a fetus to move by changing your position. Keep in mind that while these exercises won’t hurt, they might not work. However, experts often feel that if there’s a chance that the exercises might encourage a fetus to turn, they’re worth trying. These positions typically involve doing yoga-like poses. Two specific movements that your provider may recommend include:
Another thing you can try to get a fetus to change position is stimulation. Music, talking, temperature changes and light could interest the fetus. While in your uterus, the fetus can hear music, see light changes through your skin and even hear your voice as you talk. Applying cool temperatures to the top of your abdomen where the fetus’s head is could also prompt it to move away and downward. There’s no guarantee that stimulation will make the fetus move, but it’s often worth a try.
A chiropractic technique, the Webster technique, may help shift your hips and relax your uterus. Some providers even recommend acupuncture to help your body relax. For both of these techniques, you need to see a professional that your healthcare provider recommends.
Advertisement
It’s always possible that the fetus will reposition itself. In the weeks leading up to birth, there’s still time to change position. Most find their own way into the correct position before birth.
When a fetus is in a breech position or another abnormal position, your healthcare provider may suggest a C-section delivery because it’s safer. Different healthcare providers have various levels of comfort with vaginal deliveries of breech babies. Talk to your provider about the risks and benefits of different types of birth for a breech baby.
Several factors could increase the risk of a fetal position like a breech presentation. These can include:
Advertisement
Learning that a fetus is in a breech or other complicated position before birth can add to the anxiety that often surrounds childbirth. It’s OK to have concerns and questions about how a fetus’s position may affect you and it. You may have developed a birth plan during your pregnancy. These plans can be very helpful when talking to your provider about your labor and delivery experience. Your provider can help guide you through not only your ideal birth plan, but an emergency plan.
Remember, things can change quickly during childbirth. Having a C-section may not be a part of your birth plan. However, the goal is to safely deliver your child and protect your health. Talk to your healthcare provider about questions and any concerns you might have about fetal positions.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic childbirth experts coach you through every step — from labor to delivery to what to expect when you and your newborn head home.
