External cephalic version, or ECV, is a procedure pregnancy care providers use to turn a baby from a breech position to a head-down position. A provider typically does it around 37 weeks of pregnancy and improves your chances of having a vaginal birth.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
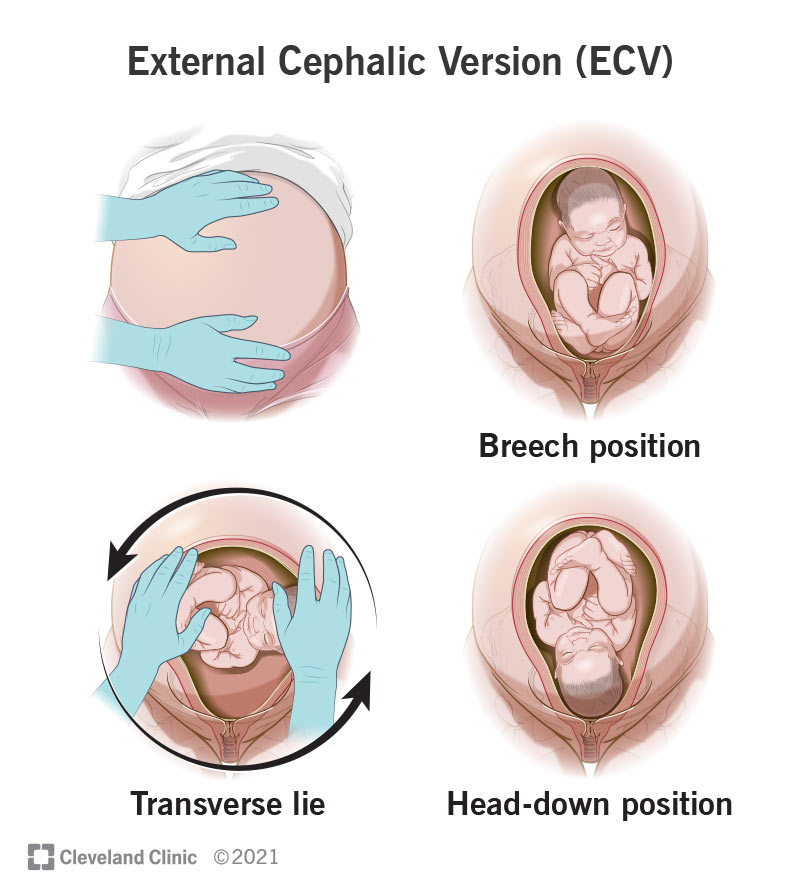
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22979-ecv)
External cephalic version (sometimes called ECV or EV) is a procedure healthcare providers will use to rotate a baby from a breech position to a head-down position. A head-down position is ideal for a vaginal delivery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
At around 36 weeks of pregnancy, most babies will turn so they’re in this position. But sometimes, this doesn’t happen.
If an external cephalic version doesn’t turn your baby and it stays breech, you’ll most likely have a C-section.
About 3 out of 100 babies are in a breech position after 36 weeks. Depending on the comfort level of your provider, they may recommend trying ECV at around 37 weeks.
Your healthcare provider (usually your obstetrician) will place their hands on your belly to turn your baby to a head-down position. The procedure is done externally by applying firm pressure to your abdomen. This pressure lasts several minutes and can cause your uterus to cramp. They don’t place their hands inside your vagina for ECV.
The whole procedure may take about two hours. This includes the time to check your baby before and after. Providers typically perform ECV near an operating room in case you need an emergency C-section.
You may feel some discomfort when pressure is applied to your belly. Many healthcare providers will give you medicine to relax your uterus. This can make it easier to turn your baby. Some healthcare providers will also offer you pain medication, but this is optional.
Advertisement
Your healthcare provider will check your medical history to see if ECV is safe. Certain factors may make it unsafe, like:
If you have a condition that prevents you from taking medications to stop contractions, you might not be able to have an ECV.
The benefit is that you can increase your chances of a safe and successful vaginal delivery. Breech pregnancies aren’t dangerous until it’s time for delivery. If you want to deliver vaginally, turning a breech baby might be your best chance at having the childbirth you planned.
Possible risks of ECV are:
Your provider will discuss the risks with you. Together, you can decide if it’s a safe option.
Yes, it can make you go into labor. ECV procedures typically happen near an operating room for this reason.
The average success rate is about 58%. This means a little more than half of all ECVs will result in a baby being turned.
Some healthcare providers may be comfortable delivering a breech baby through the vagina. It depends on their expertise and your health history and pregnancy. Speak with your healthcare provider about your delivery options if ECV doesn’t work. They might recommend other methods to encourage your baby to turn.
A C-section carries slightly more risk than ECV because it involves surgery. But it’s hard to compare them because providers use them for different reasons.
There can be a lot to think about when your pregnancy care provider suggests an ECV to turn your baby. It’s for when you want to try for a vaginal delivery, but your baby is breech — which isn’t ideal. You may have tons of questions and wonder how your birth plans will change. It can be hard not knowing what to expect. But your provider is there to answer your questions.
Discuss the procedure with them to make sure you understand the risks. Your provider will listen to you and try to make your birth plan come true. Delivering your baby healthy and safe is always their top priority.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Trying to choose where to give birth? Learn why Cleveland Clinic is the best choice to help you through each step of the labor and delivery process.
