Mesenteric ischemia is an uncommon and serious medical condition that happens when parts of your digestive system don’t get enough blood flow and oxygen. This can happen because of a blockage or circulatory issues. When it happens suddenly, this condition can be hard to diagnose and very dangerous.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
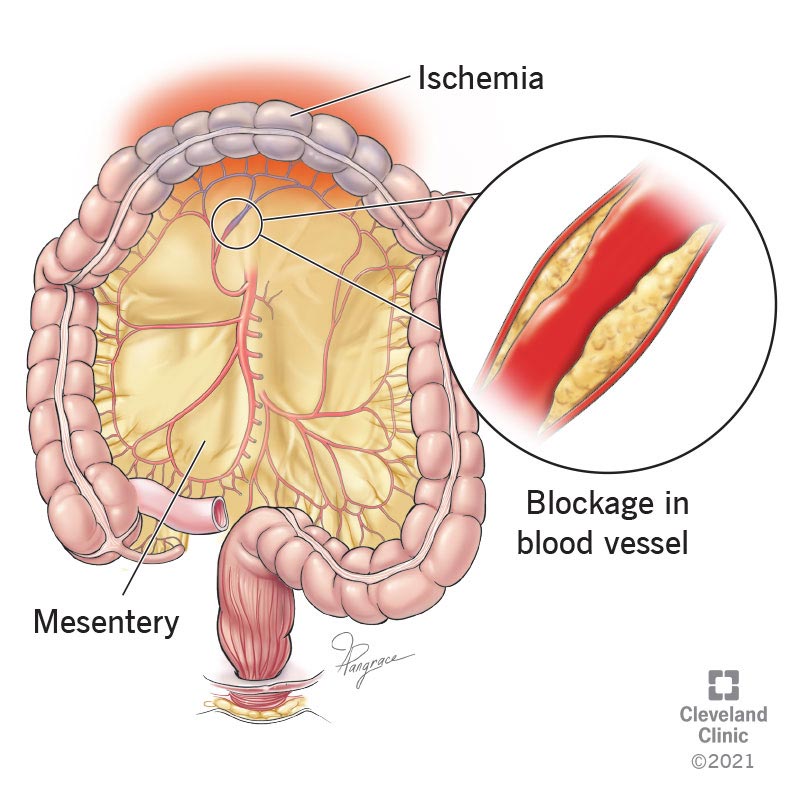
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23246-mesenteric-ischemia.jpeg)
Mesenteric ischemia is an uncommon, dangerous condition that happens when parts of your digestive system don’t get enough blood flow. This usually happens because of a blockage in your blood vessels that provide blood to those areas. This condition is more common in people who are older, especially those with cardiovascular disease or blood clotting disorders.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Without enough blood flow, the affected organs and tissues don’t have enough oxygen and can’t function correctly. If the blockage is severe enough, the affected organs and tissues may start to die. This condition is often deadly, so a quick diagnosis and treatment are very important.
The mesentery (pronounced, “mess-ent-airy”) is an organ in your abdomen (belly) that holds several other organs in place, including your small and large intestines, colon and more. The mesentery also has a network of blood vessels that supply your organs inside.
Ischemia (pronounced, “iss-key-me-uh”) is when parts of your body aren’t getting enough blood flow. Mesenteric ischemia means that the lack of blood flow is affecting your mesentery and your organs inside.
There are two types of mesenteric ischemia:
Heart attacks and strokes often happen because of blockages in critical arteries, and acute mesenteric ischemia can happen in a similar way. This usually happens because of blood clots, which cause sudden and very severe symptoms. This condition is a medical emergency that needs immediate care.
Chronic mesenteric ischemia happens more gradually, usually because your mesenteric arteries start to narrow. This condition takes longer to develop, and the symptoms usually worsen over time.
Advertisement
Mesenteric ischemia is more common as people age. It usually happens along with heart and circulation conditions, especially ones that can cause blood clots.
Risk factors for mesenteric ischemia include:
Mesenteric ischemia is a rare issue. The estimated number of cases is 1 to 2 for every 1,000 cases where someone needs hospitalization.
All of your cells, tissues and organs need a steady supply of blood and oxygen. Without that supply, they’ll start to die. What makes mesenteric ischemia so dangerous is that it affects your intestines, which contain trillions of bacteria.
Normally, those bacteria are good for you and help you digest the food you eat. But when your intestines start to die, those bacteria can spread to places they don’t belong and cause dangerous infections. That can lead to sepsis, a life-threatening condition that happens when your immune system’s overwhelming reaction to an infection ends up damaging your body, too.
Different types of mesenteric ischemia have different causes.
A waxy substance called plaque can build up inside of your arteries, causing them to harden. This condition, atherosclerosis, happens commonly with cardiovascular disease. If an area of plaque breaks open, blood clots can form there.
Clots can cause blockages in the following ways:
Non-occlusive mesenteric ischemia (NOMI), which happens without a blockage, makes up about 20% of all cases of acute mesenteric ischemia. Acute NOMI happens when blood vessels constrict, or there are spasms in the muscles lining those vessels. This can happen for several reasons.
Advertisement
Acute NOMI usually takes longer to become severe but is still dangerous.
Chronic mesenteric ischemia often happens because of circulatory diseases that cause blood vessels to narrow. This narrowing, known as stenosis, means that blood flow to your mesentery drops over time.
This condition can also happen because a blood clot forms in a mesenteric blood vessel. When this happens, the clot can grow over several days or even weeks, with symptoms getting worse as it gets larger.
While this condition isn’t usually life-threatening right away, about 40% of acute mesenteric ischemia cases happen after a person has chronic symptoms. That’s because early symptoms from narrow blood vessels suddenly become severe when a new clot blocks the narrowed blood vessels.
Advertisement
The symptoms of mesenteric ischemia vary depending on the type.
The symptoms of this condition tend to happen suddenly and include the following:
Advertisement
It’s very common for this condition to happen after you have chronic mesenteric ischemia symptoms (seen immediately below). In about half of acute cases, chronic symptoms happen first.
Symptoms of this condition can happen slowly and usually worsen over time, including:
Your doctor diagnoses mesenteric ischemia based on a combination of a physical examination, lab tests and imaging. Unfortunately, this condition is usually difficult to diagnose in its early stages. An additional challenge is that many people with this condition can’t talk or answer questions easily, especially if they’re in a lot of pain.
Many tests can help diagnose this condition, including:
A physical examination is where your doctor looks, feels and listens for signs that might mean you have a medical problem. With mesenteric ischemia, doctors can find signs in the following ways:
Physical exams might not turn up major indicators until this condition is very advanced. That means this condition can take longer to diagnose, which is part of why it’s so dangerous.
Several lab tests can help diagnose mesenteric ischemia. The tests will look for changes in your blood, especially the amount of oxygen in it and your blood’s clotting ability. The tests will also look for signs that your immune system is reacting to an infection. Other tests will show if your blood contains chemical markers that appear because of damaged or dying cells and tissues.
The best way for healthcare providers to diagnose mesenteric ischemia is to see where there’s little or no blood flow. Multiple imaging tests make that possible:
Mesenteric ischemia is treatable and reversible when it’s caught early enough.
The first priority is always to restore circulation as quickly as possible. Because mesenteric ischemia becomes more dangerous over time, healthcare providers may recommend surgery more quickly.
After restoring blood flow, the next priority is checking to see if there’s any damaged or dead tissue. In cases where sections of your intestine or colon are dead because they didn’t have enough blood flow, removing those sections is the only way to fix the damage and prevent life-threatening complications.
The likely treatments and procedures vary depending on the type of mesenteric ischemia and the location of its cause.
The most effective treatment for acute mesenteric ischemia is surgery. That’s because your surgeon can directly access and remove any existing clots and widen some narrow blood vessels. They can also place a stent, a support frame device that holds a section of blood vessel wide open.
In cases where it isn’t possible to restore blood flow directly, your surgeon can take a section of blood vessel from another place in your body and use it to create a bypass. That bypass restores blood flow by making a detour around a previously blocked area.
After restoring blood flow, your surgeon can check nearby tissue for signs of damage. If they find dead or damaged areas, your surgeon can remove them and repair the surrounding area so it can function normally in the future. In many cases, this involves a second surgery because it can take up to two days before some dead or damaged tissue is visible.
The likely medications and other supportive therapies usually include:
While this is a subtype of mesenteric ischemia, surgery isn’t always necessary to correct this problem (and it usually isn’t helpful early on). That’s because NOMI usually involves blood vessels that constrict and narrow without an actual blockage.
The key with NOMI is to treat whatever’s causing those vessels to constrict and prevent it from happening again. This may mean stopping prescription medications or recreational drugs that caused those blood vessels to tighten up. If NOMI is caused by another illness, such as sepsis, treatment of that illness will improve blood flow to the mesentery as well.
If NOMI also involves the narrowing of blood vessels, a catheter-based procedure known as balloon angioplasty may help. This procedure involves inserting a catheter into a major blood vessel and steering that device to the affected area. Once there, your healthcare provider inflates a balloon on the tip of the catheter, widening the affected blood vessel.
Other likely treatments include:
Chronic mesenteric ischemia may need some different treatments, depending on why it happens. But many of the possible treatments are the same as with acute mesenteric ischemia.
Surgery for this issue is common, especially when it involves a slow-growing clot or blood vessels that have become too narrow. It’s also more likely to happen when a person has internal bleeding, infections or sepsis, or other dangerous complications. Bypass surgery is also possible when other options can’t restore blood flow.
Balloon angioplasty and other catheter-based procedures are often considered with this condition. In many cases, healthcare providers will recommend catheter-based procedures over surgery whenever possible. That’s because surgery is harder on your body, and it’s easier to recover from a catheter procedure.
Medications that are likely with this are mostly the same as with acute cases. Clot-busting medications are also common when clots don’t move and grow into blockages.
The complications and side effects of this procedure depend on the treatments that you receive. Your healthcare provider is the best person to tell you the specific possible side effects and complications that are most likely for you.
In general, the following complications are possible with mesenteric ischemia:
Complications that are possible with surgery for mesenteric ischemia include:
Nutrition problems are possible after the removal of parts of your small intestine. Losing sections of your small intestine means it’s harder to absorb nutrition from food. Many people who have this problem, known as short bowel syndrome, need special types of nutrition like a feeding tube.
If you have mesenteric ischemia, you need immediate medical attention (especially if you have the acute type, which happens suddenly). If you have chronic mesenteric ischemia, you should care for this condition according to your healthcare provider’s instructions and guidance. You shouldn’t try to care for this condition on your own, as it can turn into a life-threatening emergency.
With quick diagnosis and treatment, most people will start to feel better when blood flow to the affected area improves. Others will likely start to feel better within days or weeks.
For those who undergo surgery, it usually takes longer for them to feel better and recover. That’s because surgery is a more intense procedure and recovery takes time.
Unfortunately, mesenteric ischemia in any form is a difficult condition to diagnose. Waiting for a diagnosis can delay treatment, and when treatment doesn’t happen quickly, acute mesenteric ischemia is often deadly. The death rate for the acute version of this condition is between 50% and 80%, especially when there are delays in treatment. When treatment happens in under 12 hours from when the blockage started, the death rate can be as low as 14%. Chronic mesenteric ischemia can also have long-term negative effects, either because of the risk of follow-up blood flow problems or nutrition difficulties.
People with mesenteric ischemia also have a much higher risk of other ischemia-related conditions. These include heart attack, stroke, pulmonary embolism and more. Follow-up visits with your healthcare provider are very important to avoid long-term problems and reduce your risk for other life-threatening conditions.
Acute mesenteric ischemia is a short-lived condition, as it’s usually deadly. Chronic mesenteric ischemia can take days or even weeks to develop. However, treatment for this condition — especially fast treatment — can usually resolve the condition within hours.
Your healthcare provider can best explain the likely timeline of your recovery. Depending on the severity of your case and the treatments involved, many people can return to most or all of their usual activities within days or weeks. In more severe cases, especially those involving surgery, it may take longer.
There are several things you can do to reduce your risk of developing mesenteric ischemia. Most of them involve preventing or avoiding conditions that can make mesenteric ischemia more likely.
The things you can do include:
Most of the actions that will help prevent mesenteric ischemia are the same steps that can reduce your risk. Unfortunately, there will be some cases — especially those involving injuries or conditions where your blood clots too easily — where prevention isn’t possible.
After you have mesenteric ischemia, it’s important to follow your healthcare provider’s guidance. They’re the best person to guide you on how you can take care of yourself and avoid further problems. In general, you should do the following:
You should see your healthcare provider if any symptoms of mesenteric ischemia return, change or start to get worse. You should also ask them about specific warning signs or symptoms that indicate you need to call their office or seek medical care.
You should seek immediate medical attention if chronic symptoms suddenly change or get worse, or if you have any symptoms of acute mesenteric ischemia. Acute symptoms include:
Mesenteric ischemia can be a frightening condition, especially when it happens suddenly. Fortunately, modern medicine has made great advances when it comes to diagnosing and treating this condition quickly. There are also several steps you can take to reduce your risk of developing this condition or having it return after you recover from it. The best things you can do are to know and manage your risks. Your healthcare provider can be a big help for both of those goals and can help you recover from this condition or avoid it entirely.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Plaque in your blood vessels can cause tingling, pain and numbness. Cleveland Clinic’s experts treat circulatory problems, including peripheral artery disease.
