ALS (amyotrophic lateral sclerosis) is a neurodegenerative condition that affects how nerve cells communicate with your muscles. It leads to muscle weakness that gets worse over time. Symptoms can affect how you move, speak and breathe. ALS treatment includes therapies and medications to manage symptoms and slow the progression of the disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Amyotrophic lateral sclerosis, or ALS, is a neurodegenerative disease that targets the nerve cells (neurons) in your brain and spinal cord. It affects your muscle control. Symptoms worsen over time.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You might notice muscle weakness and muscle twitching that affect your ability to walk independently, reach for objects, chew food and talk. ALS eventually causes your muscles to waste away (atrophy). Atrophy can make it harder to breathe and may lead to life-threatening outcomes.
Amyotrophic lateral sclerosis was formerly known as Lou Gehrig’s disease. Gehrig was a famous baseball player in the 1920s and 1930s who had the condition.
An estimated 5,000 people in the United States receive an ALS diagnosis each year.
Although there’s no cure, treatments are constantly improving. The right combination may slow the progression of the disease and improve your quality of life.
There are two types based on their cause:
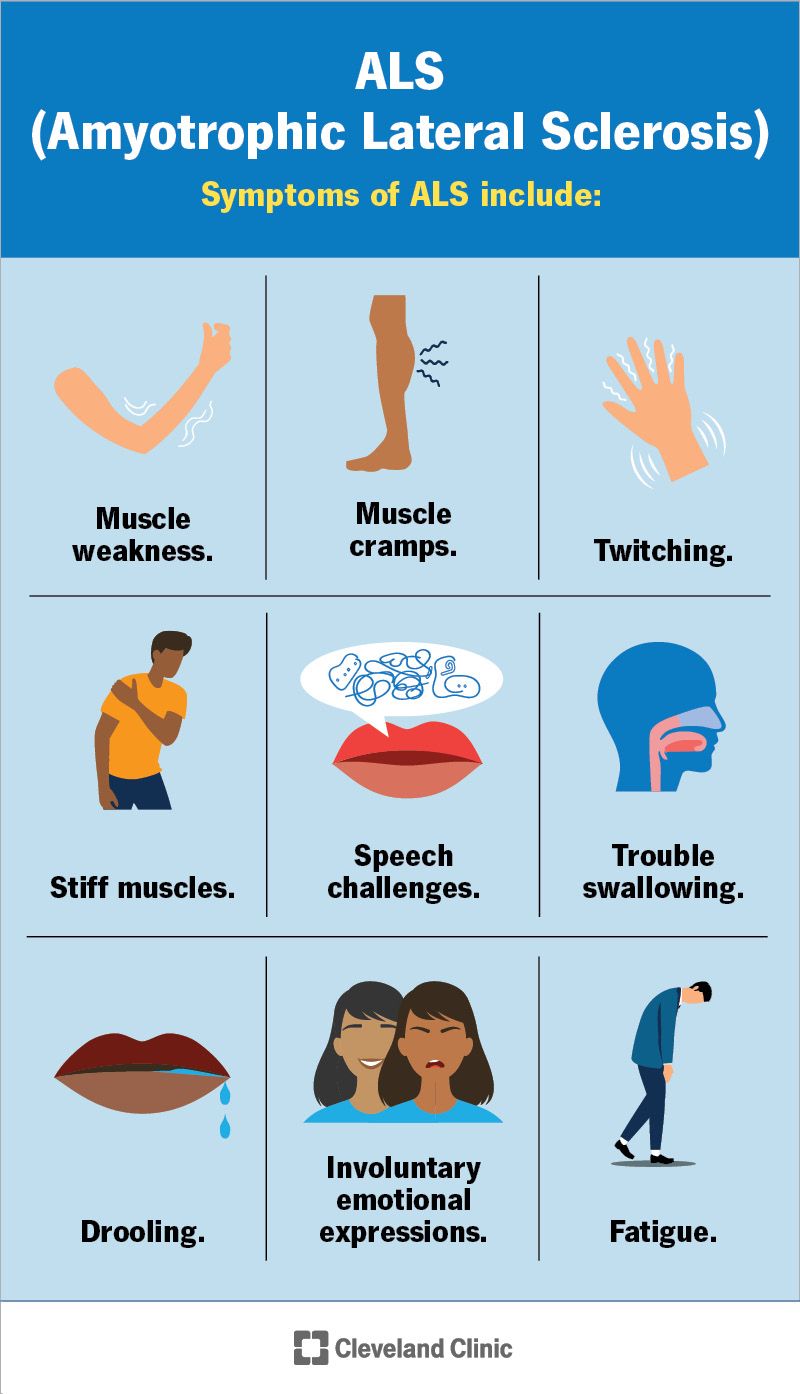
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16729-amyotrophic-lateral-sclerosis-als)
Amyotrophic lateral sclerosis symptoms include:
Advertisement
Early symptoms are usually muscle weakness or stiffness in your arms and legs, as well as trouble with speech and swallowing. These can make everyday tasks like writing or eating more challenging. Over time, symptoms typically spread throughout your body. The speed at which symptoms progress varies from person to person.
As symptoms get more severe, you may have trouble breathing, standing or walking. You might experience significant weight loss. Contact your healthcare provider if symptoms worsen, and seek emergency care if you’re having trouble breathing.
Researchers don’t know what causes amyotrophic lateral sclerosis. They believe it’s a combination of the following factors:
What researchers do know is that the disease targets motor neurons. These regulate your voluntary movements, like talking, chewing, moving your limbs and breathing.
Your neurons communicate with your muscles to tell them to move. ALS disrupts communication, like bad phone reception. The messages sent from neurons to muscles break up and don’t get through clearly. This eventually causes the call to end. As a result, neurons can’t take any new calls, causing you to experience symptoms.
Some types of amyotrophic lateral sclerosis are genetic. You can inherit genetic changes that cause ALS from your biological parents. Inherited ALS isn’t common, though. Sometimes, genetic changes happen randomly, without a history in your biological family.
Risk factors for amyotrophic lateral sclerosis include:
This condition will shorten your life expectancy as symptoms get more severe. Learning about this disorder and dealing with it every day can take a toll on your mental health. You may feel overwhelmed, lost, hopeless or stressed. As a result, many people diagnosed with ALS also develop depression and anxiety.
While you’ll be working with a number of providers for your physical health, make sure you take care of your emotional health as well. Talk to your care team or a mental health provider for help.
A healthcare provider will do a physical exam, neurological exam and testing to make a diagnosis.
Advertisement
An ALS diagnosis doesn’t happen immediately. You’ll likely schedule several office visits to see your provider or referring physicians. Your provider will order multiple tests to learn more about your symptoms and how they affect your body. There are a lot of conditions that have similar symptoms to ALS, so different exams and testing are necessary for an accurate diagnosis.
You’ll need several tests to confirm a diagnosis, including:
No treatment can reverse ALS damage. But it may help delay the progression of symptoms and make you more comfortable.
Your care team might recommend the following:
You may need different types or more treatment options as the disease progresses. In addition, supportive care is available to meet your needs so you can live as comfortably and independently as possible for as long as possible.
There are four medications approved by the U.S. Food and Drug Administration (FDA) to treat amyotrophic lateral sclerosis:
Advertisement
Other medications are available to manage your symptoms. This could include medications for muscle cramps, stiffness and excess saliva production, pain and mental health challenges.
Your provider might recommend different types of therapy or rehabilitation, including:
With ALS, it can be hard to eat and drink enough to meet your body’s needs. Swallowing difficulties may cause weight loss and make it harder to get essential vitamins and minerals.
A dietitian can help you follow a meal plan that avoids hard-to-swallow foods and provides the right balance of calories, fiber and fluids. Nutritional counseling supports healthy eating, and a nutritionist can suggest alternatives as swallowing becomes more challenging.
Advertisement
If needed, a feeding tube may reduce the risk of choking or pneumonia from food or liquid entering your lungs.
As ALS progresses, breathing may become difficult. Noninvasive ventilation (NIV), delivered through a mask over your nose and mouth, can make breathing more comfortable. You may start using it at night and eventually need it full time.
Over time, you might need mechanical ventilation with a respirator to help inflate and deflate your lungs. Let your care team know if you feel short of breath, especially when lying down or being active. They’ll discuss options to make breathing easier.
Contact your healthcare provider if you:
ALS can make breathing difficult. Symptoms of breathing problems that mean you should contact your provider include:
These symptoms can lead to respiratory failure, where you aren’t breathing in enough oxygen to support your body. This is life-threatening. Contact emergency services if you have trouble breathing.
On average, the life expectancy after an ALS diagnosis is three to five years. An estimated 30% of people live five years or more, and 10% to 20% live at least 10 years. Your life expectancy can vary from these statistics, so talk to your healthcare provider to learn more about your situation.
The outlook for ALS is poor because of how it affects motor neuron function. Your prognosis depends on how quickly the damage happens. While no treatment can reverse this damage, your provider can offer options to slow symptom progression.
There’s no available cure for ALS at this time.
If you have ALS, you may want to join a clinical trial. These studies help researchers develop new treatments and better understand the disease.
There’s no proven way to prevent ALS. Research is ongoing to learn more about the causes and risk factors to help create prevention methods in the future.
Receiving an amyotrophic lateral sclerosis (ALS) diagnosis can spark a lot of questions and emotions. You may wonder, “What caused this and why?” You might even feel overwhelmed and frustrated by not being able to do routine things as well as you used to, like brushing your hair, enjoying a meal or maintaining a conversation with loved ones. This can lead to depression and anxiety, especially as you start to see symptoms progressively get worse.
No matter where you are or what you’re feeling, your care team is available to help you. Treatment for ALS is improving, and new treatment options are being studied and tested at this very moment. While there isn’t a current cure, treatment options can delay how fast symptoms progress and give you more time to spend with the people you care about.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you learn you have ALS, you want the best care possible. Cleveland Clinic’s here to support you and help you manage your condition.
