If your cornea changes shape and becomes more like a cone than a dome, your vision is likely to be less sharp. Treatments range from glasses or contact lenses to a cornea transplant. In most cases, keratoconus has no definite cause.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
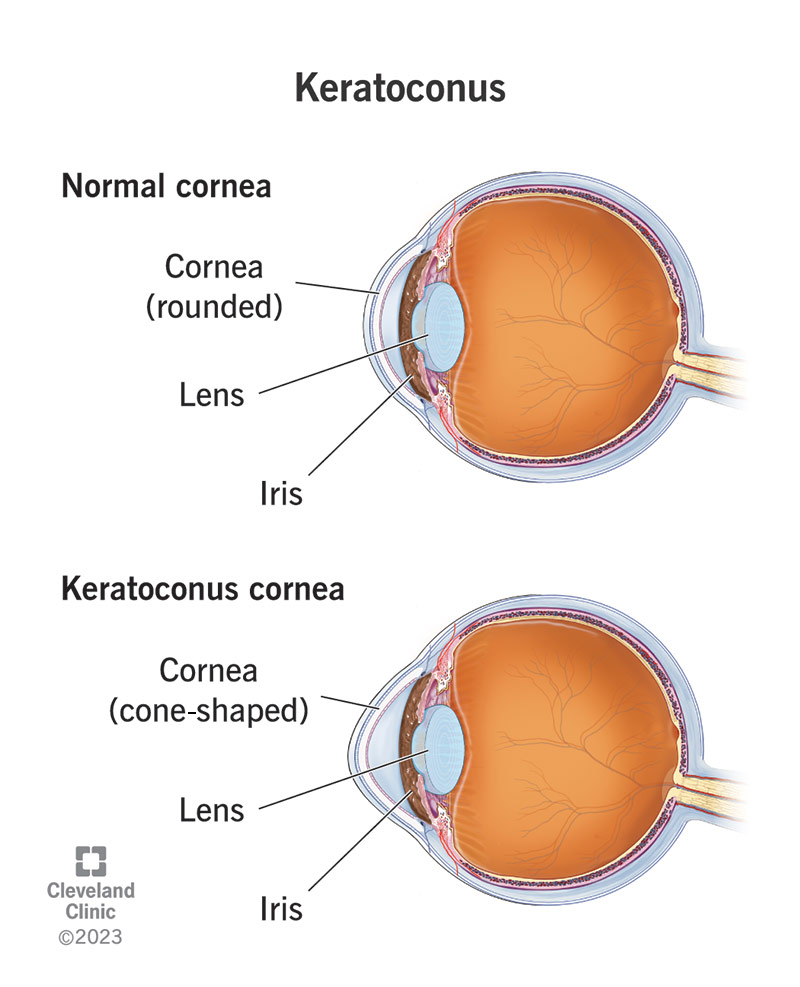
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/keratoconus)
Keratoconus is a condition of the eye in which the normally rounded cornea bulges outward into a cone shape. The cornea is the clear, central part of the front surface of the eye. It protects your eye and helps you focus for clear vision. You pronounce keratoconus as care-ah-ta-KO-nus.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Eye care providers normally find keratoconus during your teenage years or your 20s and 30s, but it can also start in childhood. In some cases, a provider will diagnose a mild case of keratoconus at a later age. The changes in the shape of the cornea occur over several years but happen at a more rapid rate in younger people.
Keratoconus changes vision in two ways:
One estimate says that keratoconus develops in 50 to 200 of every 100,000 people.
The main symptoms of keratoconus include:
The cause of keratoconus is largely unknown. Some studies have found that keratoconus runs in families, and that it happens more often in people who have certain medical conditions.
Advertisement
In most cases, you don’t have an eye injury or a disease that leads to keratoconus. People with keratoconus tend to rub their eyes a lot, which may cause the condition to develop more rapidly.
Keratoconus has a link to certain conditions that may also be associated with chronic eye rubbing. These conditions include:
Potential complications of keratoconus include:
Your eye care provider will begin by asking you about your medical and family history and your symptoms. They’ll then do a comprehensive eye exam. They may also order one or more of the following tests:
There are several methods for treating keratoconus, depending on how severe the condition is. Your eye care provider can help to decide which, if any, of these treatments may help you. Treatments include eyeglasses, contact lenses, implantable ring segments, corneal crosslinking and cornea transplant.
In the early stages of the disease, you can correct vision with normal eyeglasses or soft contact lenses. As keratoconus gets worse, eyeglasses may not correct your vision because of the amount of irregular astigmatism. You may need a special type of hard contact lens.
Corneal crosslinking uses ultraviolet (UV) light treatment that may slow or stop the keratoconus from getting worse. In this procedure, you also receive local anesthesia. Your provider puts drops of a drug containing riboflavin (vitamin B2) into your eye for up to 30 minutes. Then, your provider exposes your eye to an UV light for up to 30 minutes. The purpose of corneal crosslinking procedure is to strengthen the bonds between your cornea’s collagen fibers and surrounding proteins. This can help keep your cornea’s shape from getting steeper.
INTACS® are small devices your provider inserts into your cornea to improve vision or make it easier to fit you with contact lenses. Your provider performs this procedure while you’re under local anesthesia (drops numb your eye). Then, your provider creates channels in the cornea and inserts the rings into these channels. The rings help to flatten the cornea and partially correct the cone shape the keratoconus causes.
Advertisement
Your provider may suggest that you have a cornea transplant if you have keratoconus that’s advanced. They’ll replace your diseased cornea with corneal tissue from a human donor. Usually, people with keratoconus have better vision after the transplant, but it may take more than a year for vision to stabilize. Some people may still need a specialty contact lens after the transplant to get their best vision.
Potential complications from corneal cross-linking include:
Potential complications from INTACS include:
Potential complications related to cornea transplant include:
Potential complications or side effects from glasses or contact lenses are rare, but can happen. Let your provider know if you have any redness or discomfort in your eyes.
Your recovery time for keratoconus treatment varies by the type of treatment. It can take days for some treatments and much longer for others.
With treatment, the outlook for someone with keratoconus is good.
If your vision or prescription is different in each eye, you might find yourself dealing with balance issues. Speak to your provider about this. They’ll help you find a solution.
Advertisement
Every person is different. Some people have mild cases of keratoconus that don’t progress. Other people have cases that do progress. No one can predict what will happen in every case.
Untreated keratoconus can lead to permanent vision loss. The changes to the cornea make it difficult for your eye to focus with or without eyeglasses or standard soft contact lenses.
In addition, keratoconus can be dangerous if you have laser vision correction surgery such as LASIK because the surgery can make keratoconus worse. If you’re thinking about this kind of surgery, your eye surgeon will do an exam to see if you’re a candidate. If you have even a small degree of keratoconus, you shouldn’t have LASIK, unless your provider specifically recommends it.
No, you can’t prevent keratoconus. If you have a condition associated with keratoconus, you may be able to reduce your risk by doing your best to avoid rubbing your eyes.
You should always contact your eye care provider when you have changes in vision. If you have keratoconus, you’ll probably need to see your provider on a regular basis. Keep your appointments.
Go to an emergency room (ER) if:
Advertisement
You may want to ask your provider questions, such as:
Keratoconus can affect your vision but shouldn’t stop you from living a fulfilling life.
In general, having keratoconus doesn’t mean that you’re legally blind. However, if you have a more advanced case of keratoconus, your vision loss might be severe enough to make you legally blind.
Having an eye condition like keratoconus can be worrying, but your eye care provider is on your side. There are treatments for keratoconus. Your provider will work with you to find the best treatment for you. Knowledge is your friend, so be sure to ask questions and talk freely about your condition, and what you need and want to be able to live your best life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s ophthalmologists and optometrists have the highest training available. We provide exams, vision correction and care for many eye conditions.
