Avascular necrosis, also known as AVN or osteonecrosis, happens when your bone tissue starts to die. This may happen if something keeps blood from flowing to your bones. AVN weakens your bones and joints. It may make your joints collapse. Treatment is surgery to restore blood flow or replace damaged joints.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
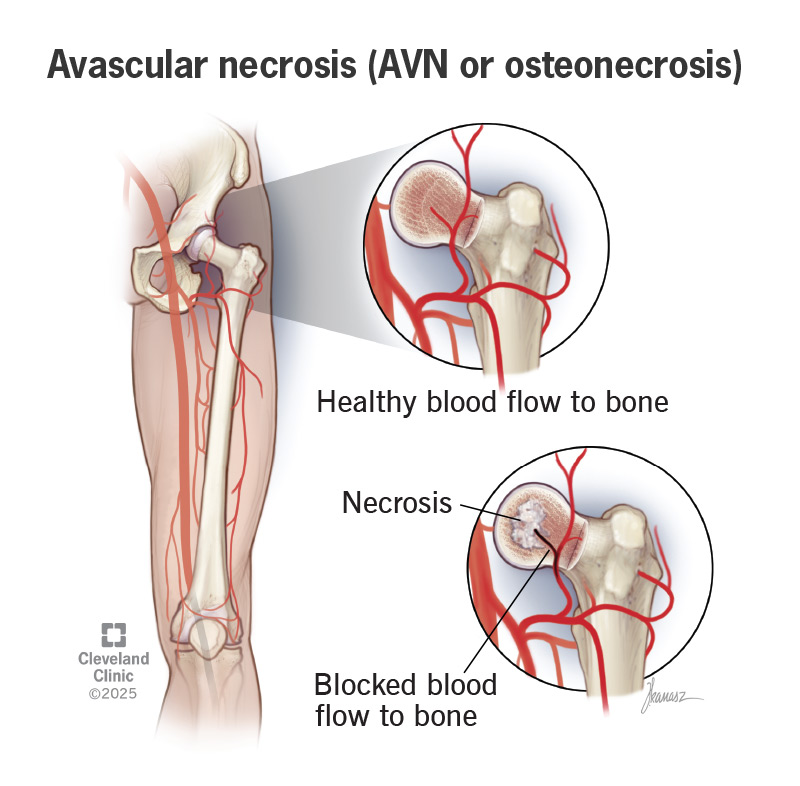
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/avascular-necrosis-avn-osteonecrosis)
Avascular necrosis, also known as AVN or osteonecrosis, is a disease that may happen if something blocks the flow of blood to bone tissue near your joints. Your bone tissue dies when it doesn’t receive enough blood. Without treatment, this condition can get worse so that dead bone eventually breaks down or crumbles. Osteonecrosis near or in your joints may cause them to collapse. The disease may affect any bone in your body. But it most often affects:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Avascular necrosis can worsen over time. Early diagnosis and treatment may keep the disease from causing more damage to your bones.
AVN symptoms develop over weeks or months. Symptoms that may appear over time include:
Bone fractures, certain diseases and lifestyle activities that affect your blood flow may cause AVN. Your skeletal system needs a steady flow of blood to make healthy bone tissue to replace dying bone tissue. Without blood flow, your skeletal system can’t produce new bone tissue fast enough. The dying bone starts to crumble and collapse.
Healthcare providers may classify AVN as traumatic or nontraumatic avascular necrosis. Traumatic AVN happens when you break a bone or dislocate a joint. Hip fractures or dislocations are a common cause.
Nontraumatic AVN may happen if you have a medical condition or treatment that keeps blood from flowing to your bone tissue. Nontraumatic avascular necrosis often affects the same bones on both sides of your body. That means osteonecrosis in your right shoulder may affect your left shoulder. Medical conditions or treatment that may lead to AVN include:
Advertisement
You may develop this condition if you smoke, drink a lot of alcohol, or use prednisone or other corticosteroids for a long time.
A healthcare provider will ask about your symptoms and your medical history, including specific medical treatments that may lead to AVN. They may do an MRI to look for osteonecrosis signs.
A healthcare provider will recommend treatment based on your bone damage, including:
Surgery for osteonecrosis may be:
Avascular necrosis can affect your quality of life. But it isn’t life-threatening and won’t affect how long you’ll live. People who have avascular necrosis can also develop severe osteoarthritis. If that’s your situation, you may need surgery, including joint replacement.
You should contact a healthcare provider if you:
Avascular necrosis can turn everyday activities into painful chores. It can make it hard for you to walk, bend or straighten your arms or legs. Talk to a healthcare provider if you have pain in your bones or joints that doesn’t go away. That ache in your bones may be a symptom of avascular necrosis.
Early diagnosis and treatment can slow AVN down and reduce its impact on your quality of life.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From sudden injuries to chronic conditions, Cleveland Clinic’s orthopaedic providers can guide you through testing, treatment and beyond.
