Lower back pain is very common. It often results from a strain (injury) to muscles or tendons in your back. Other causes include arthritis, structural problems and disk injuries. The pain often gets better with rest, physical therapy and/or medication.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Lower back pain affects the lumbar region of your spine or back. It can result from many different injuries and conditions. Most often, the cause is an injury to muscles or tendons in your back.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Nearly everyone experiences lower back pain at some point in their lives. The pain can range from mild to severe. For most, it’s temporary. But long-lasting (chronic) lower back pain is also common — up to 23% of adults worldwide have chronic lower back pain. In extreme cases, lower back pain can make it difficult or impossible to walk, sleep, work or do everyday activities.
Given how common it is, it may be hard to tell if you should be worried about your lower back pain. Trust your gut and reach out to a healthcare provider if something feels off — or if the pain keeps you from going about your usual activities.
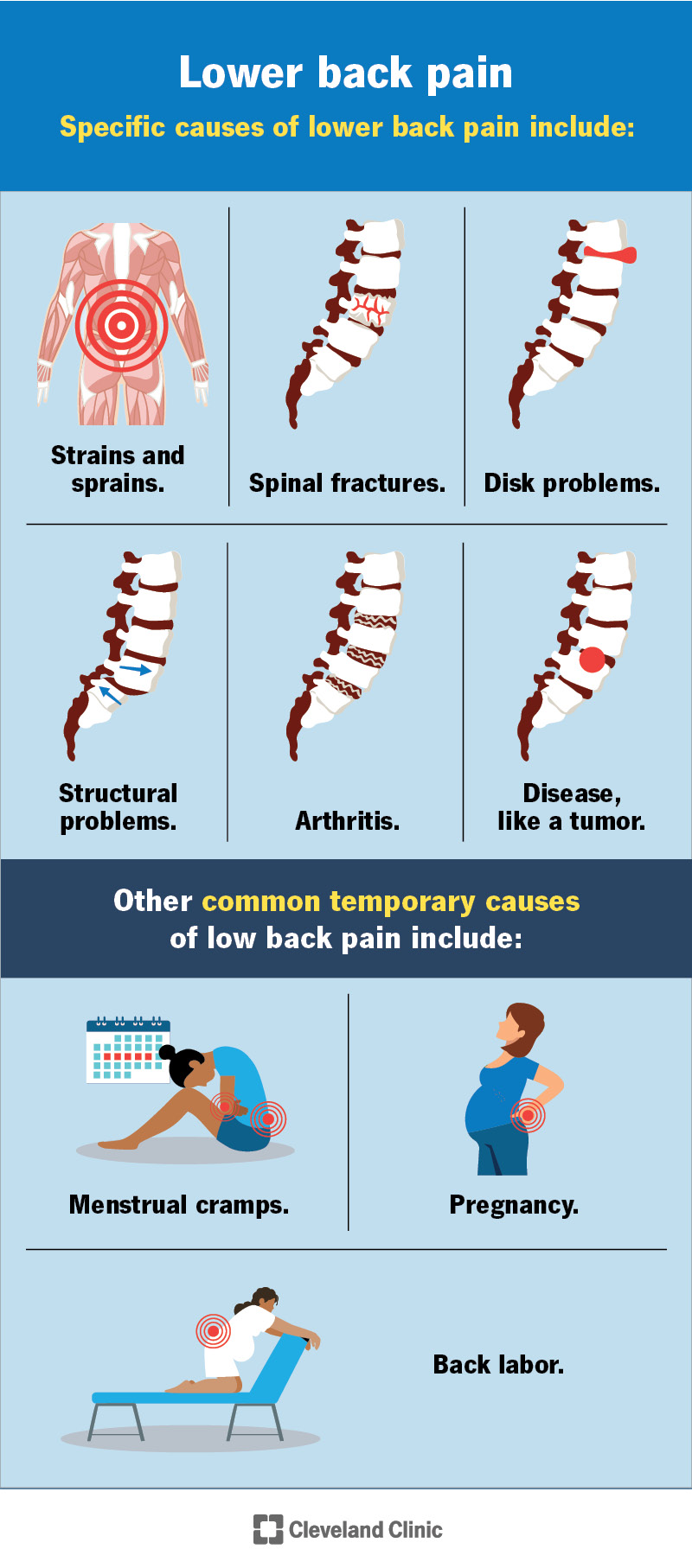
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/7936-lower-back-pain)
Lower back pain can involve a wide spectrum of symptoms. Lower back pain may:
Other symptoms of lower back pain can include:
Advertisement
If you have severe pain and/or lower back pain that keeps you from doing daily activities, reach out to a healthcare provider.
Many injuries and conditions can cause lower back pain. This kind of pain is so common because your lumbar (low back) vertebrae (bones) do a lot to support your body, including:
With all these important functions, any issue with the structures in your lower back can lead to pain. Specific causes of lower back pain include:
Other common temporary causes of lower back pain include:
Some people are more likely to have lower back pain than others. Risk factors for lower back pain include:
Advertisement
Your healthcare provider will ask about your symptoms and medical history and do a physical exam. Your provider may recommend a variety of tests to check your spine for injuries and assess your health in other ways. Tests may include:
Because there are so many possible causes of low back pain, it may take time to find the correct diagnosis.
Many cases of mild to moderate lower back pain get better with rest, ice and over-the-counter (OTC) pain relievers. After a few days of rest, you should be able to get back to your normal activities. Staying active increases blood flow to the area and helps you heal.
Advertisement
If your back pain is severe and/or happens after a traumatic accident, like a fall, you should seek medical treatment as soon as possible.
Other treatments for lower back pain depend on the underlying cause, severity and how long you’ve had pain. They may include:
Advertisement
It may take time to find the best treatment for you, especially if you have chronic lower back pain. Your provider will be by your side throughout the process.
The prognosis (outlook) for someone with lower back pain depends on several factors, including:
Your healthcare provider will be able to give you a better idea of what to expect based on your unique situation. Most people with back strains and sprains recover and don’t have long-term health issues. But many people will have another episode within a year.
Some people have chronic back pain that doesn’t get better after several weeks. People with degenerative conditions such as arthritis and osteoporosis may have symptoms that get worse over time. Surgery and other treatments are often effective at helping people with a range of injuries and conditions live with less pain.
Not all causes of lower back pain are preventable. But you can take some steps to avoid injuries that cause lower back pain, including:
Certain symptoms that happen alongside lower back pain can be warning signs of something more serious. You should see a healthcare provider right away if you have lower back pain and any of these symptoms:
While not as urgent, it’s a good idea to see a provider soon if you have lower back pain and any of these:
Millions of people experience lower back pain. Stiffness, pain and limited movement can have a major impact on your quality of life. Know that you don’t have to struggle through pain. Talk to a provider if lower back pain doesn’t go away or if you’re unable to do the activities you enjoy. Several treatments can help relieve pain, help you move better and let you get more out of life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Low back pain can be a constant interruption in your daily life. Cleveland Clinic’s experts can help craft a treatment plan to help you find relief.
