Macular degeneration is primarily an age-related retinal condition. There are two types of macular degeneration — wet and dry. You may lose central vision, but you aren’t likely to lose all of your vision. There are treatments, but there isn’t a cure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
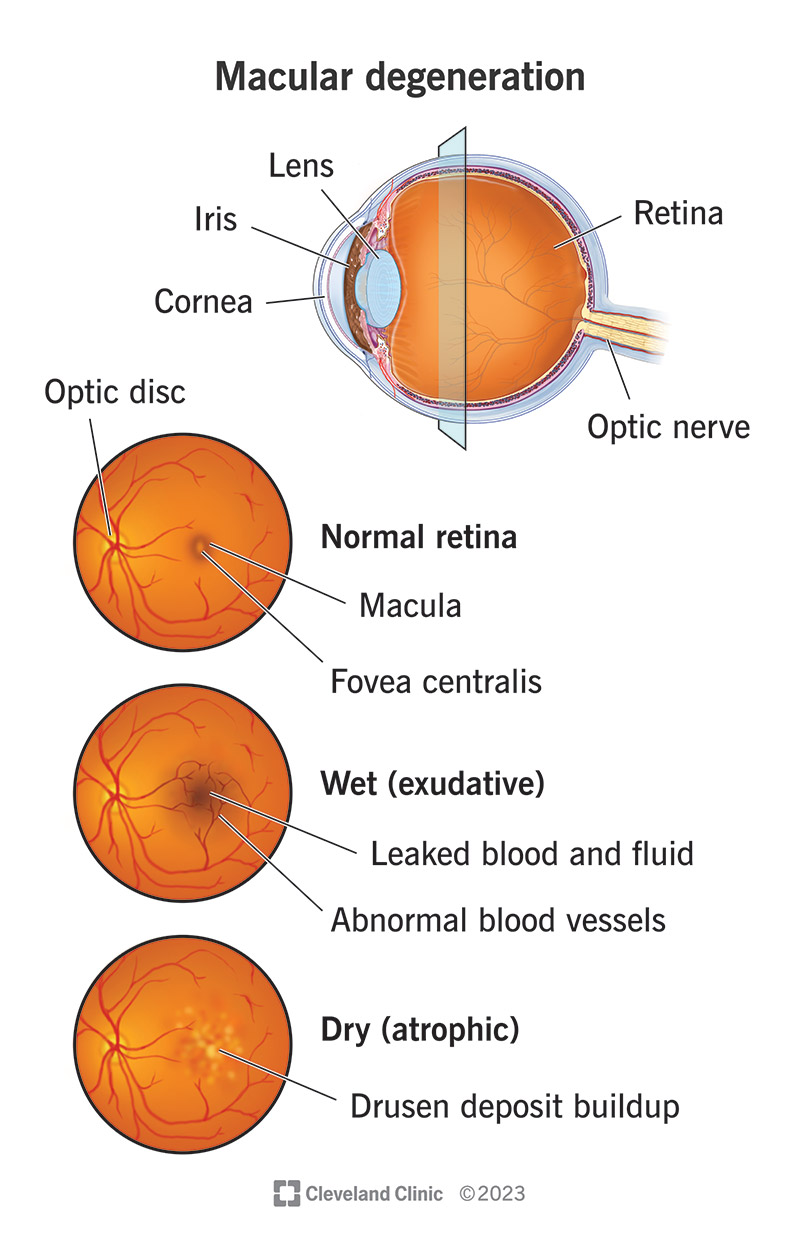
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/macular-degeneration-2)
Macular degeneration is an eye disease that affects central vision. This means that people with macular degeneration can’t see things directly in front of them. This common age-related eye condition mostly occurs in people over the age of 50.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Macular degeneration affects your macula, the central part of your retina. Your retina is in the back of your eye and controls central vision. People with macular degeneration aren’t completely blind. Their peripheral vision (ability to see things off to the sides) is fine.
Macular degeneration may develop in one eye or both eyes with different levels of severity.
Almost 20 million U.S. adults have macular degeneration. Globally, the prediction is that 288 million people will have the condition by 2040.
In the U.S., macular degeneration is a leading cause of vision loss in people who are 60 and older.
As the term “age-related macular degeneration” (AMD) implies, macular degeneration is more likely to occur as you get older. However, people can develop macular degeneration at younger ages because of several factors.
In addition to age, risk factors for macular degeneration include:
There are two types of macular degeneration: dry and wet.
Nearly 90% of people with macular degeneration have the dry form. It develops when tiny yellow protein deposits called drusen form under your macula. The built-up deposits dry and thin your macula.
Advertisement
Vision loss with the dry form of macular degeneration tends to occur gradually. Most people don’t completely lose central vision. In some cases, the dry form can change to the wet form.
Wet (exudative) macular degeneration occurs when abnormal blood vessels develop under your retina and macula. The blood vessels leak blood and fluid. “Exudative” is a term that refers to how the fluids ooze.
Because of fluid buildup, a bulge forms in your macula. You may see dark spots in your center of vision. About 10% of people with macular degeneration have the wet form. This type is more severe. It can quickly lead to total loss of central vision.
Dry macular degeneration has three stages. Often, symptoms like vision loss aren’t evident until the late stage. However, your eye care provider can see signs when doing an exam.
Wet macular degeneration is already at an advanced stage.
Macular degeneration can be an inherited eye disease. But it also develops in people with no family history of the disease. Macular degeneration occurs when the macula at the back of your eye starts to waste away for unknown reasons. Getting older is a factor in age-related macular degeneration.
Non-age-related macular degeneration may be associated with:
The macula helps send images from your eye’s optic nerve to your brain. If you have a damaged macula, your brain can’t understand or read the images that your eyes see.
Many people with macular degeneration don’t have symptoms until the disease progresses. You may experience:
Macular degeneration rarely causes symptoms in its early stages, so annual eye examinations are very important. They’ll help your provider find the disease early and start treatments when they’re most effective.
During an eye exam, your eye care provider checks for changes to your retina and macula. Your provider may order one or more of these tests:
Advertisement
There’s no cure for macular degeneration. Starting treatments early can slow the progression of the disease and make symptoms less severe. Even with successful treatments, symptoms often return. Depending on the disease type, treatments include nutritional supplements, medications, photodynamic therapy (PDT) and laser therapy.
The Age-Related Eye Disease Studies (AREDS and AREDS2) found that a combination of vitamins and minerals might slow the progression of dry AMD. AREDS supplements include these ingredients:
The first version of the supplements contained the antioxidant beta-carotene, but it raises the risk of lung cancer in people who smoke and people who used to smoke. In the newer version, zeaxanthin and lutein are the antioxidants.
There are drugs that treat but don’t cure wet AMD. They include anti-vascular endothelial growth factor (anti-VEGF) injections. They block the production of VEGF, which is a protein that produces new blood vessels. Your provider, generally a retina specialist, will numb your eye before giving you a shot into the vitreous (intravitreal injections). Anti-VEGF shots can sometimes improve your vision.
Advertisement
These drugs include:
During photodynamic therapy (PDT), your eye care specialist uses a combination of an injectable light-sensitive drug and a laser to destroy extra blood vessels in your eye. Your provider may combine PDT with anti-VEGF shots.
During this treatment, your provider will use a laser to seal and destroy the leaking blood vessels. This was actually the first treatment for wet AMD.
Providers don’t use laser photocoagulation and PDT as often as they once did due to the development of anti-VEGF injections.
Treatments for wet AMD carry some risk of complications, including:
Losing your central vision can make it challenging to do certain tasks. Depending on the extent of vision impairment, you may not be able to:
Severe AMD may lead to you being legally blind.
Changes in your lifestyle can lead to depression and anxiety. Some people with AMD experience Charles Bonnet syndrome, a condition that causes visual hallucinations.
Advertisement
Not everyone who has macular degeneration experiences significant vision loss. With dry age-related macular degeneration, vision loss can happen slowly and take a long time to occur. Because the condition can affect just one eye, you may not notice any change in vision.
Even if you’re legally blind, you might be able to see better if you:
You can take these steps to lower your risk of macular degeneration:
You should call your healthcare provider if you have macular degeneration and experience:
If you have age-related macular degeneration (AMD), you may want to ask your healthcare provider:
Age-related macular degeneration (AMD) is the leading cause of vision loss in older adults. Although AMD doesn’t cause complete blindness, the loss of central vision can make it harder to do everyday tasks. Dry macular degeneration, a condition that causes gradual vision loss, is the most common form. Taking nutritional supplements may slow the disease. Wet macular degeneration can cause rapid vision loss and may lead to legal blindness. Your eye care provider can offer treatments that may help preserve vision. You also may benefit from wearing eyeglasses or using magnifying devices to read. You can also ask your provider to give you information on supportive services.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
If you see dark or blank spots when reading or looking at people, Cleveland Clinic can help. We offer personalized macular degeneration diagnosis and treatment.
